The humanity has been facing the pandemic of coronavirus infection COVID-19, officially recognized by the World Health Organization in March 2020 for more than a year and a half. As of August 2021, more than 210 million cases have been recorded since the virus began to spread. All over the world, vaccination against COVID-19 is being actively carried out, treatment methods are being finalized, scientists are developing new approaches that will make it possible to more effectively fight the pandemic in the future.
Countries around the world are in different stages of the pandemic, and many states are now entering the phase of dealing with the consequences of COVID-19. This applies not only to economic and political problems, but also to the health of citizens. People who have had the coronavirus infection now need rehabilitation. Many affected by the disease complications may now be at risk for long-term health deterioration and even disability. Accurate data on the possibility of deterioration and disability are not yet available, but it is clear from early studies that all patients need rehabilitation, which should be carried out from the very beginning – from the acute stage of the disease.
Below we will review the currently known information about the virus that causes the coronavirus infection, mention the clinical features of the disease and dwell in detail on the methods of rehabilitation therapy, which is of key importance in the recovery of patients.
SARS-CoV-2 –infectious agent of COVID-19
Infectious agent of COVID-19 is a previously unknown SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus-2). It is called the second because it is very similar in structure to the SARS-CoV virus that caused the outbreak of atypical pneumonia in 2002.
Studies of all aspects related to SARS-CoV-2 are still at the initial stage. New articles are published every few days, and sometimes, articles published a few months ago are no longer relevant. In the absence of evidence on rehabilitation from the coronavirus infection, the recommendations essentially based on studies are performed in connection with the epidemic of atypical pneumonia. The epidemic of atypical pneumonia has similar characteristics to COVID-19.
Virus SARS-CoV-2 has several modes of transmission: It is believed that the disease is most easily transmitted by airborne droplets, transmission by fecal–oral and contact mechanisms is possible. The main infection source is a sick person, including those in the incubation period. Airborne transmission occurs when coughing, sneezing and talking at a close (less than 2 meters) distance. The contact route of transmission occurs during handshakes and other types of direct contact with an infected person, as well as through food products, surfaces and objects contaminated with the virus.
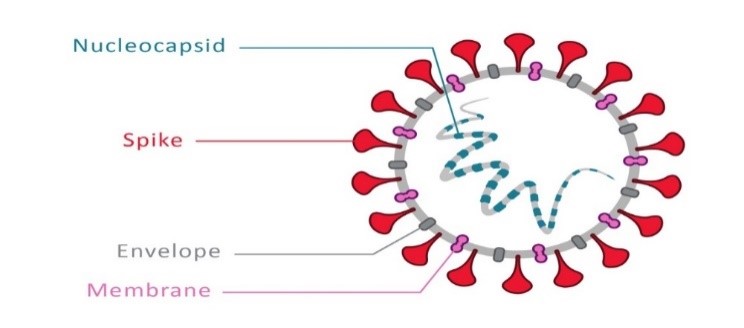
In the image above, you can see that the virus is flanked by claviform spikes due to which it resembles the solar corona (hence the name). Once in the human body, the virus with the spikes “attaches” to the cells of the respiratory tract, gastrointestinal tract, vascular cells, penetrates within and begins its reproduction cycle. After some time, an infected cell reaches a critical level and dies, releasing new copies of the virus.
High activity of the virus and cell death attracts the immune forces of the body: leukocytes (neutrophils), monocytes, lymphocytes. Their task is normally to stop the spread of infection. For that, immune cells with biologically active substances trigger various reactions, which can result in symptoms such as:
- temperature rise
- weakness,
- loss of appetite,
- pain in muscles and joints,
- headaches.

covid-19 symptoms
The above pathogenesis of the disease causes known symptoms:
- Viral pneumonia is the main manifestation of COVID-19. It develops when the virus infects the alveolitis – lung cells that are normally responsible for breathing and gas exchange. As a result of the death of these cells, lung function decreases. There are symptoms such as:
-
- cough,
- dyspnea,
- chest pain,
- as well as the above phenomena caused by the immune response (fever, muscle pain, etc.)
- Loss of smell (anosmia) and / or taste occurs due to pathological processes in the nasal cavity, as well as when the olfactory pathways in the brain are involved. Such symptoms are highly specific and may appear alone, without other signs of the disease.
- Dizziness, movement disorders, loss of balance – are not so common symptoms of coronavirus infection, which, nevertheless, require close attention and rehabilitation.
- Digestive disorders as nausea, vomiting, diarrhea are quite common in patients. Such manifestations are related to the involvement of cells lining the gastrointestinal tract by the virus.
- Fatigue, weakness, loss of strength, apathy
- Joint pain, muscle pain

Covid-19 complications
The coronavirus infection can result in such complications as:
Impairment of cognitive functions (thinking, memorization, concentration of attention).
Often, people who have had a severe infection, especially if they have been ventilated, experience a cognitive decline. This problem may disappear spontaneously within a few weeks after recovery, but in some patients, it may continue for a longer period and require rehabilitation measures.
Decrease of respiratory functions, including respiratory failure.
Cardiovascular diseases, for example, myocarditis.
Reduced physical activity, fatigue lead to the need for rehabilitation of the musculoskeletal system.
Inactivity and lack of physical activity during the period of coronavirus infection negatively affects our health. We are less physically active, we go out less, and there are many people who leave the house very rarely. Lack of physical activity is a serious health hazard.
In the article by the World Health Organization published in March 2020, it warns that lack of exercises after a period of COVID-19 increases the risk of osteoporosis, diabetes, cardiovascular problems, cancer, dementia, and being overweight.
! An Italian study conducted in May 2020 shows that even a few days of sedentary lifestyle is already enough to reduce muscle mass, affect the neuromuscular system, lead to changes in insulin levels, reduced aerobic capacity, fat accumulation and changes in inflammation levels in body. In the elderly persons (60-85 years, average 67 years), the consequences of a 10-day rest are severe for health. Studies point to a significant decrease in leg muscle strength, decreased endurance, and difficulty with physical exercise such as climbing stairs.
The study concludes that moderate exercise, along with a 15-20% reduction in caloric intake, is necessary to preserve the cardiopulmonary, neuromuscular, metabolic and endocrine systems.
Neurological complications
Inflammation of blood vessels leads to the formation of blood clots and can cause a stroke. As a result, people are left with paralysis, movement disorders, sensory problems, problems with speech and swallowing. In fact, significant impairment of functioning and independence.
There is evidence for the development of multiple sclerosis
An excessive immune response can cause brain cell death and lead to psychiatric symptoms such as confusion, disorientation, and even psychotic attacks.
As part of this immune response, encephalitis can develop, leading to headaches, confusion, and fatigue. More advanced and serious signs include seizures, tremors, hallucinations, and memory problems.
The percentage of people suffering from neurological problems after coronavirus disease is still not entirely clear. In addition, the mechanism of neurological damage is still unclear. Despite this, it is very important to pay attention to the development of neurological signs.
People with neurologic deficit need to pay special attention to the gradual rehabilitation at all levels. Neurological rehabilitation, respiratory rehabilitation and very moderate activity with a gradual increase in load are key to the correct formation of the rehabilitation process.
Syndrome of general (chronic) fatigue (asthenic syndrome)
Patients who have undergone COVID-19 are characterized by a constant feeling of fatigue, weakness, loss of strength. From a medical point of view, asthenic syndrome is the body’s reaction to a condition fraught with loss of energy resources. It is characterized by such symptoms as muscle weakness, drowsiness, absent-mindedness, anxiety, mood swings, suspiciousness, weight loss, decreased libido, irregular menstruation, increased sensitivity to light, sound, etc.
Studies after the epidemic of atypical pneumonia show that 60% of recovering patients report fatigue even a year after the disease.
40% reported chronic fatigue even after 4 years
27% of recovering patients met criteria for chronic fatigue syndrome
There is a constant and inexplicable fatigue, leading to serious impairment of everyday social functioning.
The syndrome is accompanied by sleep disturbances, muscle pain, memory and concentration disorders, headaches, joint pain, dizziness, nausea, loss of appetite, night sweats and other symptoms that are also observed in patients with coronavirus The syndrome is accompanied by sleep disturbances, muscle pain, memory and concentration disorders, headaches, joint pain, dizziness, nausea, loss of appetite, night sweats and other symptoms that are also observed in patients with the coronavirus.
One of the syndrome signs is the post extertional malaise, a phenomenon in which symptoms worsen after physical or even cognitive exertion. Aggravation appears between 12-72 hours after exercise, there is a marked deterioration in function, and resolves in 24 hours. A similar phenomenon is observed in the recovery period after the coronavirus infection. It is very important to avoid reaching the state of maximum effort and overload during rehabilitation in order to prevent the development of this phenomenon.
The treatment of chronic fatigue syndrome has not been conclusively studied. There is a theory based on the “conservation of energy”. Patients have less available energy, and therefore they need to modify their lifestyle in accordance with their abilities and physical capabilities, find a balance between activity and rest. In case of intolerance to physical exertion, there is a tendency to inactivity, and this can affect the physiological body condition, therefore, while recovering, it is necessary to form an exercise and training program of a very low level with a gradual load increase. For example, start with stretching, gradually move to a walk for a few minutes, swimming, focus on rest between daily activities, save energy on unnecessary tasks, etc.
A study published in August 2020 in the British Medical Journal offers instruments to diagnose and treat people who report symptoms lasting more than 3 months. It emphasizes the strong need to monitor vital signs and, guided by the appearance of “red flags”, immediately seek the help of a rehabilitation physician. As for physical activity, this article recommends gradually increasing activity while maintaining a healthy lifestyle.

Rehabilitation after COVID-19
Rehabilitation is defined as “a set of activities aimed at reducing the risk of disability and optimizing the functioning of patients with health problems while interacting with the environment”. At the moment, it is certainly known that rehabilitation has an extremely positive effect on the health of patients who have had a severe form of COVID-19. In rehabilitation process, it is of great importance to start “at the bedside”, during the disease itself.
For each individual case, rehabilitation methodology is carefully prepared by a team of specialists, consisting of a rehabilitation physician, a physiotherapist, an attending physician and other medical specialists in concomitant diseases. Factors to consider when developing a rehabilitation plan for patients who have had COVID-19 include:
- Degree of damage to the lung tissue.
- Damage to other organs and systems due to COVID-19.
- Concomitant diseases not related to COVID-19 (for example, frequent comorbidities for patients with the coronavirus infection are hypertension, coronary heart disease, diabetes mellitus).
Due to the course and possible complications of the disease, there are 4 main directions of rehabilitation that should be mentioned.
Video: “Rehabilitation after COVID-19 Coronavirus Infection”
Exercises for post-COVID rehabilitation. The first (1) direction: rehabilitation of the respiratory system
For additional information about the recovery process after COVID-19 Coronavirus Infection, you can watch a video demonstrating exercises and rehabilitation recommendations.
Respiratory rehabilitation
It is recommended not to start respiratory rehabilitation too early to avoid the disease aggravation or excessive virus spreading. When the disease passes into the subacute phase, and a patient’s condition improves, they begin breathing exercises techniques. Respiratory rehabilitation aims to:
- reduction of shortness of breath,
- clearing the airways,
- respiratory muscle training, chest mobilization,
- exercises for chest stretching.
MAIN PRINCIPLE OF RESPIRATORY GYMNASTICS
EXHALATION IS TWO TIMES LONGER THAN INHALATION
It is important to remember to gradually increase the load. To control the dynamics, specialists regularly measure the level of oxygen saturation in the blood, monitor the respiratory rate and pulse. Some patients are prescribed inhalers and breathing simulators.
Breathing exercises and the use of other methods of respiratory rehabilitation allows you to saturate the lungs with oxygen, improve their blood supply, help restore damaged cells and increase the elasticity of the lung tissue. Manual therapy methods, in turn, allow you to restore muscle strength and mobilize the chest. Daily implementation of the exercises and procedures indicated by specialists will help reduce the risk of respiratory diseases, increase the overall tone of the body, increase the vital capacity of the lungs and improve gas exchange, thereby restoring effective breathing.
For patients with shortness of breath, specialists recommend body positions in which breathing is facilitated: lying on the side with a raised headboard, sitting with the torso forward, standing with the torso forward, standing with an adequate back support.
Cardiovascular rehabilitation
One of the complications of coronavirus infection is myocarditis. This is an inflammation of the cardiac muscle tissues which leads to such symptoms as:
- Cardiac arrhythmias – a feeling of cardiac failure (the heart “freezes”, “turns”, “jumps”)
- Heart pain (aching or paroxysmal)
- Lowering blood pressure by reducing cardiac output
A frequent manifestation of myocarditis is the temperature increase up to subfebrile figures.
In advanced cases of myocarditis, such complications as cardiosclerosis (replacement of the cardiac muscle tissue with connective tissue not able to contract normally) and heart failure occur. In order to prevent complications, it is necessary to carry out rehabilitation measures aimed at restoring cardiac functions.
In the acute phase of myocarditis, it is recommended to limit physical activity, so rehabilitation begins with an improvement in the patient’s well-being and clinical values. According to a specialist’s decision, light physical exertion is indicated with a slow and gradual increase in heart rate for a smooth restoration of cardiac functions.
Other cardiovascular disorders after COVID-19 are blood coagulation disorders. These complications are very serious, as they suggest a high probability of developing thrombosis, pulmonary embolism, strokes and organ infarctions. These disorders are treated with drug therapy prescribed by a physician, and it should be carefully observed by patients in order to restore normal balance in the vascular system.
General fatigue syndrome and rehabilitation of the musculoskeletal and muscular system
General fatigue syndrome or asthenic syndrome in rehabilitation is usually considered in combination with cognitive impairment and disorders of the musculoskeletal system. Surprisingly, for all these complications, an effective method of rehabilitation is the restoration of exercise tolerance.
Despite the feeling of impotence and weakness that is typical for the disease, a patient should regularly perform a course of exercises indicated by a physiotherapist-rehabilitation specialist. One of the most effective methods of physical rehabilitation is walking rehabilitation.
It should be taken into consideration that load should be increased gradually. After a long disease, the organ systems get used to simple actions again, you should not overload them. Specialists advise to carry out physical activity little by little, but often.
If a patient feels well, under the control of saturation and pulse, cardio and strength trainings are gradually indicated, that may be performed by each individual patient. Until the restoration of respiratory and cardiac functions, the disappearance of weakness, you should refuse from using dumbbells, weights and other sports equipment should be neglected.
Frequent rest between trainings is required. The criteria for stopping physical activity are:
HR > 100 bpm, BP <90/60 mmHg or BP> 140/90 mm Hg,
SpO2 <95%, Temperature > 37.2°C.
Physical exercises can help restore such functions as thinking, memorization, concentration can be helped by physical some exercises. Among other activities, exercises for the brain are effective. New hobbies or activities, jigsaws, puzzles, reading contribute to the formation of new neural connections and the gradual restoration of the lost brain functions.
Physiotherapy methods are effective for resolving the asthenic syndrome. Physiotherapy exercises, manual therapy, massage eliminate muscle tension, tone up the body, eliminate fatigue and improve blood circulation, giving any patient strength. We should not forget about psychotherapy, which is an integral part of the treatment of chronic fatigue, along with the above methods.

Dizziness and Rebalancing
Balance and motor disorders, dizziness in case of the coronavirus infection are associated with damage to the cerebellum and vestibular apparatus, which are responsible for the normal maintenance of these processes. The restoration of the functions of the cerebellum and the vestibular apparatus after the infection should be carried out smoothly and gradually. The main treatment for dizziness and unsteadiness is vestibular rehabilitation.
Dizziness often occurs when turning the head, body – due to that, patients try to avoid such movements. Vestibular gymnastics is a set of exercises aimed, among other things, at turning the head and torso. Regular performance of such exercises helps the vestibular apparatus to adapt to changes in body position and prevent dizziness and loss of balance. Exercises can be performed while sitting on a bed, on a chair, standing. Vestibular gymnastics is based on the principle of sensory mismatch between the movements of the eyes, torso and head.
To varying degrees, post-COVID rehabilitation is necessary for everyone who has had the disease, regardless of the form of the previous disease. Patients who have had the mild disease can independently practice breathing and restorative gymnastics at home, while patients who have had the moderate disease should be controlled by a medical specialist, and vital signs should be monitored.

Check out the demo version of our exercises for post-COVID rehabilitation on YouTube.
Our website presents sets of exercises for rehabilitation after COVID-19 in the following four areas:
-
Exercises for Post-COVID rehabilitation. The first (1) direction: rehabilitation of the respiratory system.
-
Exercises for Post-COVID rehabilitation. The second (2) direction: rehabilitation of the cardiovascular system.
-
Exercises for Post-COVID Rehabilitation. The third (3) direction: rehabilitation of the vestibular system.
-
Exercises for Post-COVID rehabilitation. The fourth (4a) direction: rehabilitation of the musculoskeletal system. Physical activity, stretching, mobility and muscle strengthening. Initial stage. Starting position – lying.
-
Exercises for Post-COVID rehabilitation. The fourth (4b) direction: rehabilitation of the musculoskeletal system. Physical activity, stretching, mobility and muscle strengthening. Middle stage. Starting position – sitting on a chair or stool.
-
Exercises for Post-COVID rehabilitation. The fourth (4c) direction: rehabilitation of the musculoskeletal system. Physical activity, stretching, mobility and muscle strengthening. Advanced stage. Starting position – standing.



