The most wicked of all diseases are those that develop slowly and in the early stages of their existence can only be known by chance. Only gradually progressing, they are manifested by symptoms that at first slightly affect a person’s life, but over time become a real obstacle to vigorous activity. These diseases include Parkinson’s disease.
Main symptoms of Parkinson’s disease
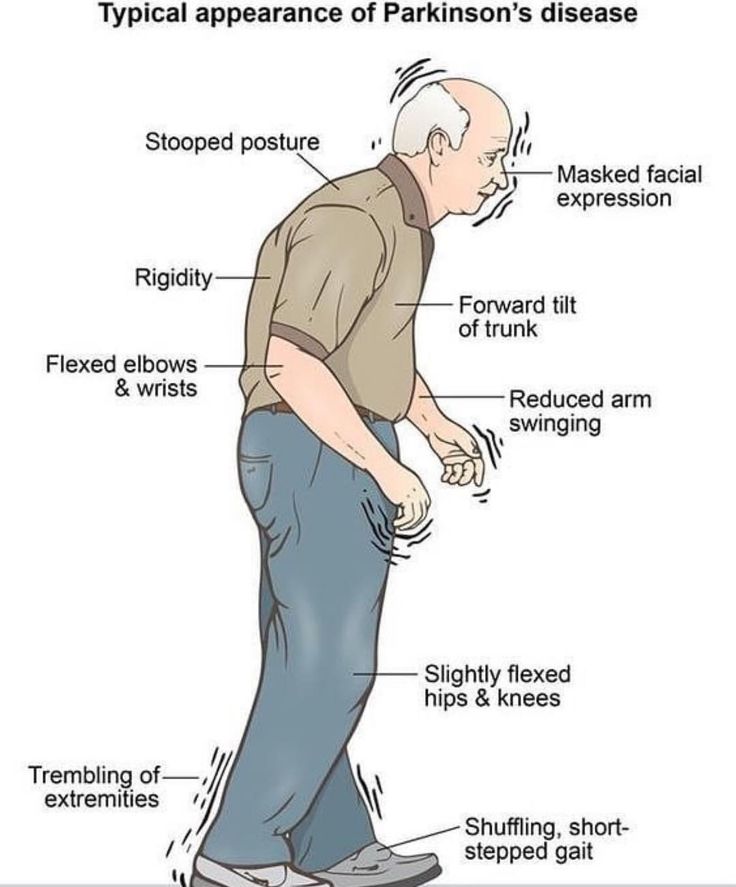
Parkinson’s disease is a slowly progressive chronic disease that occurs in people over the age of 60 due to the degeneration (destruction) of nerve cells in the brain and is manifested by the following main symptoms:
-
Tremor (trembling) in various parts of the body – head, jaw, limbs.
-
Stiffness in limbs and trunk.
-
Hypokinesia (decrease in pace and range of motion).
-
Disturbances of balance and coordination.
-
Gait disturbances and high probability of falls.
-
Hunched posture.
-
Bradykinesia – slow movements.
-
Joint pain occurring as secondary symptoms.
-
“Freezing” – the phenomenon of freezing that occurs when you begin walking.
To understand the cause of these symptoms and deal with the methods of the disease treatment, it is necessary to dwell on the features of anatomy and pathogenesis (development mechanism).
Anatomical and pathogenetic features of Parkinson’s disease
As we know, Parkinson’s disease is caused by the death of nerve cells in the brain. But what are these cells, why do they die, and how does this affect the appearance of the main symptoms?
There are several well-organized systems of neurons in the brain. Some of them are responsible for the transmission of information from our senses – touch, smell, sight, hearing, taste. The function of another system of neurons is the formation of movements. One of the links in such a system is the substantia nigra, located in the midbrain region. The development of Parkinson’s disease is associated with the death of neurons located within.
We still cannot tell why it happens. Some scientists correlate degenerative changes with the natural aging process, changes in a patient’s DNA structure sometimes can be found. Although some cases of Parkinson’s disease appear to be hereditary, and some can be attributed to specific genetic mutations, in most cases, the disease occurs by chance and is not inherited. Regardless of the source of the disease, it occurs the same way.
Parkinson’s disease risk factors
There are also risk factors:
-
Work with pesticides, salts of heavy metals.
-
Heredity.
-
Chronic cerebrovascular insufficiency.
-
Head injury.
-
Administration of some narcotic drugs (MPTP).
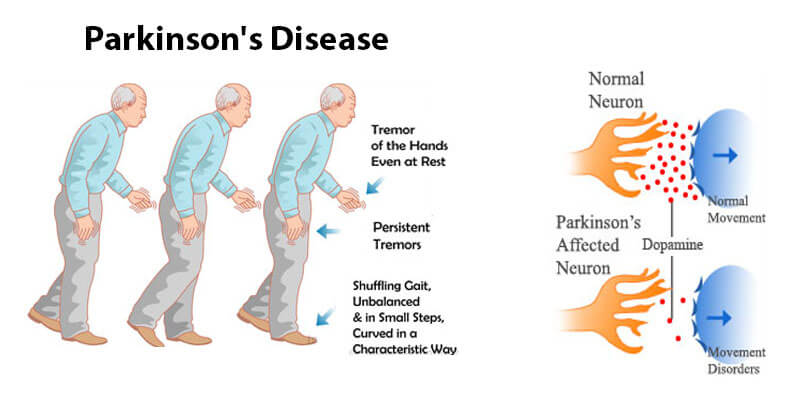
Parkinson’s disease, neuronal process, receptors, synapse, dopamine, neuronal process at Parkinson’s disease, neuromediator deficiency
Neurons in the substantia nigra normally produce dopamine. This neurotransmitter helps neurons in the midbrain connect with neurons in the higher parts of the brain (cortex) and start motor activity. Therefore, when dopamine-producing cells die, a neurotransmitter deficiency occurs. Impulses are transmitted to the superior parts of the brain “worse”, it becomes more difficult to initiate motor activity. Here, the first of the main symptoms of Parkinson’s disease occurs – hypokinesia (decrease in the pace and range of movements).
Tremor and Gait Change
Another function of the dopamine system in the brain is to maintain the accuracy of movements, their coordination. Therefore, when the neurons of the substantia nigra are affected, such symptoms as tremor (involuntary trembling, which is most pronounced at rest and disappears when moving) and muscle stiffness (also manifested by hunchback and almost unemotional facial expression).
Due to the aforesaid, patients with Parkinson’s diseases show two more typical symptoms such as the change in gait – patients take short steps, keep their arms bent, do not swing them (mining gait), and postural instability, leading to balance disorders and falls.
Other symptoms of Parkinson’s disease can include depression and other emotional changes, dementia, difficulty swallowing, chewing, and speaking, urination problems or constipation, and sleep disturbances.
As mentioned above, Parkinson’s disease is a slowly progressive disease. The above symptoms do not appear at once, but begin with barely noticeable manifestations that increase over the years and form a complete clinical picture. All patients have an individual rate of progression of symptoms. In some cases, the disease goes unnoticed and is regarded as a natural aging process: for example, patients may feel a slight trembling in the limbs or have difficulty getting up after a long sitting.
Often, symptoms can appear only on one side of the body, and only over time, the other side will be involved in the pathological process.
Treatment and rehabilitation
Currently, no method exists that would help to cure completely Parkinson’s disease. However, various means and methods of rehabilitation are used that slow down the disease progression, partially eliminate its symptoms and improve the quality of life of patients.
First of all, a medical specialist prescribes an individual course of drug therapy (most often, Levodopa is a precursor of dopamine), which is aimed at eliminating dopamine deficiency in the nervous system and improving the initiation of motor activity, reducing tremor and muscle stiffness.
In rare cases, if drugs fail, surgery is indicated (DBS = deep brain stimulation). During the surgery, a device is implanted that directly sends signals to those parts of the brain where the system of neurons of the substantia nigra cannot deliver them (due to a neurotransmitter deficiency).

How to improve the quality of life of the patients with Parkinson’s disease
One of the most effective ways to improve the quality of life of the patients with Parkinson’s disease are rehabilitation methods, including:
- Motor rehabilitation – physiotherapy exercises, complexes of gymnastic exercises, Nordic walking, etc. Methods of motor rehabilitation allow to increase the pace and range of movements, increase endurance, coordination and balance.
- Improvement of cognitive functions – training of memory, reaction time, verbal activity.
- Social support and psychotherapy
- Occupational therapy – maintaining and restoring daily skills
- Speech correction therapy – in Parkinson’s disease, speech becomes quiet, monotonous, slow, and swallowing disorders develop. Speech therapy methods can reduce the severity of these symptoms.
Video: “Rehabilitation of the patients with Parkinson’s Disease”
Set of exercises 1 for Parkinson’s Disease: improving joint mobility and increasing body flexibility
For additional information about Rehabilitation of the patients with Parkinson’s Disease you can watch a video demonstrating exercises and rehabilitation recommendations.
physiotherapy and rehabilitation
Thus, rehabilitation methods for Parkinson’s disease, prescribed by a qualified specialist in physiotherapy and rehabilitation, combined with drug therapy, can significantly improve the quality of life of patients, improve motor and cognitive functions, and reduce the symptoms of the disease.
To maintain the health of patients with Parkinson’s disease, it is important to combine different operations and activities. Every day, you can combine and vary as follows – strength training, walking training, exercise bike training, training to improve joint flexibility, improve posture and balance. Of course, it is important to combine training with daily activities and, therefore, to practice the functions used in everyday life: sitting, getting up (from bed, from a chair), mobility in bed, etc.
The process of rehabilitation and treatment of patients with Parkinson’s disease, of course, depends on the disease stage (primary or progressive). But regardless of this, the process of developing and forming a rehabilitation program should take into account four main areas:
-
Improve joint mobility and increase body flexibility
-
Strengthening the musculoskeletal and muscular system, endurance
-
Improving the coordination and “composition” of any movement – dividing it into components.
-
Improve balance, gait and fall prevention
As recent studies have shown, for patients with Parkinson’s disease, it is important to form a rehabilitation plan based on a stepwise, gradually changing training rhythm and increasing exercise difficulty. Constancy and monotony in the choice of physical activity and activity is not recommended.

Check out the demo version of our sets of exercises for Parkinson’s Disease on YouTube
Our website presents the following sets of exercises for the rehabilitation of the patients with Parkinson’s Disease:
-
SET OF EXERCISES №1 FOR PARKINSON’S DISEASE: IMPROVING JOINT MOBILITY AND INCREASING BODY FLEXIBILITY
-
SET OF EXERCISES №2 FOR PARKINSON’S DISEASE: STRENGTHENING OF THE MUSCULOSKELETAL AND MUSCULAR SYSTEM, ENDURANCE
-
A SET OF EXERCISES №3 FOR PARKINSON’S DISEASE: IMPROVING THE COORDINATION AND “COMPOSITION” OF MOVEMENT – DIVIDING IT INTO COMPONENTS
-
A SET OF EXERCISES №3 FOR PARKINSON’S DISEASE: IMPROVING THE COORDINATION AND “COMPOSITION” OF MOVEMENT – DIVIDING IT INTO COMPONENTS



