Gait disorders are a common consequence of past injuries of the spine, spinal cord, and extremities. Injuries such as compression fractures of the vertebrae, destabilization of the spine, damage to the ligaments and joints of the lower extremities inevitably lead to compensatory changes, the rehabilitation of which sometimes takes a long time. In this article, we will discuss the causes that lead to gait disorders and how to correct them.
Physiological basis of gait and its disorders
Walking, by definition, is a complex, locomotor, symmetrical, cyclic movement associated with the repulsion of the body from the supporting surface and its movement in space.
Walking cycle
Walking cycle is determined from the moment the left (or right) foot touches the ground until the moment it touches the ground again.
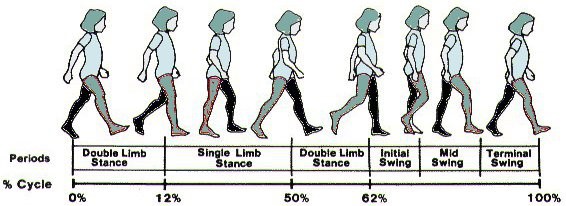
A walking cycle is usually divided into several “phases” (sections) that refer to the left (or right) foot during the walking cycle. This initial division basically divides the walking cycle into two parts:
Stance phase (foot contact with the ground) is about 60% of the walking cycle, this phase begins with the initial contact of the foot with the ground and until the foot is released from the ground. Throughout this phase, the foot is in contact with the walking surface and carries the weight of the body).
Swing phase of the foot is about 40% of the walking cycle, from the moment the foot leaves the ground to the point where it touches it again, throughout this phase the foot does not touch the ground and does not carry load.
The faster you walk, the shorter the STANCE PHASE and the longer the SWING PHASE. For example: when walking fast, the swing phase will increase to 60%, and the advance phase will decrease to 40%, and vice versa, when walking slowly, the advance phase will increase to 70% of the walk cycle, and the transition phase will decrease to about 30% of the walk cycle. It should be noted that when walking fast, the pace of walking increases, so walking cycle has a short period of time. Therefore, in the transition to brisk walking, both the tread (walk) phase and the transition phase will be shortened, but the transition phase will be negligible, and the walking phase will be reduced very significantly.
The correct walking pattern should be economical and energy efficient. A movement according to the usual, physiological pattern of walking should occur as follows: – foot, starting from the heel, through the lateral surface of the ankle (foot), and from there back to the center of the foot through the metatarsal bones – to the big toe.
For a normal, from a physiological point of view, gait, there are a number of necessary conditions:
-
The body should be in a stable upright position
-
The support should be evenly distributed first on one, then on both legs
-
The joints of the lower limb (hip, knee, ankle) should be in a normal physiological state.
-
Correct posture also influences the physiological gait.
If one of the above links is impaired, gait disorders occur. There are many reasons for these impairment. Here we will review in more detail the impairment caused by injuries, as well as mention other relevant factors.
Classification of gait disorders
Causes of gait disorders are classified into neurological, orthopedic, psychiatric, and other medical conditions. Based on the causes of occurrence, types of gait disorders are as follows:
Atactic
Atactic a gait in which the body is significantly “loosened” to the sides. It is characteristic of lesions of the structures of the central (cerebellum) and peripheral nervous system. For example, ataxia can occur after a traumatic brain injury, with multiple sclerosis, after viral diseases: HIV, COVID-19, etc.
Hemiparetic
This type of gait disorder is characterized by squinting steps in a circular motion. The cause of such disorders can be the consequences of a stroke, birth trauma, brain abscess, brain tumors.
Perineal
Perineal is characterized by sharp movements of the foot forward. Such a gait is a consequence of diseases of the nervous system: multiple sclerosis, poliomyelitis, etc.
Paraspastic
Paraspastic is typical for elderly people with chronic hypertension, as well as for patients with cerebral palsy, vitamin B12 deficiency.
Hypokinetic and hyperkinetic
Hypokinetic and hyperkinetic is most often are the result of damage to the nervous system.
Idiopathic senile
Appears due to age-related deformities of the musculoskeletal system, it is characterized by short steps and caution when walking, caused by fear of falling and joint stiffness.
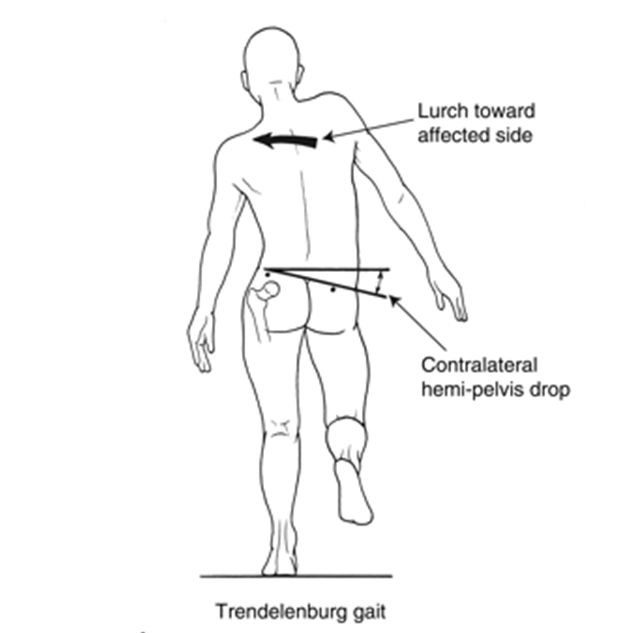
Duchenne’s lameness
“Duck” walking with insufficiency of the hip bone, hip injuries, congenital dislocation of the hip, muscle underdevelopment.
“Intermittent claudication”
Intermittent claudication – with insufficiency of the cardiovascular system and deterioration of the blood supply to the lower extremities.
Disorders
The most common causes of gait disorders are injuries of the musculoskeletal system. Disorders such as injuries of the spine, limbs, joints and ligaments require the close attention of a qualified specialist and the prompt initiation of appropriate correction and recovery programs.
Spine injury
The spine is an axial structure that maintains the correct position of the body. Any pathological changes in this structure lead to numerous disorders, including gait disorders.
Vertebral compression fracture
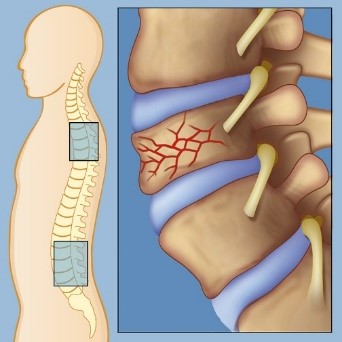
Vertebral compression fracture is a common cause of gait disorders. Such fractures occur when falling from a height on the head, legs or buttocks.
The main symptom of the fracture is a sharp pain in the affected area at the time of injury. The pain is usually very strong, a person reflexively strains the muscles to alleviate the condition and reduce discomfort, remains motionless for some time. In addition to the general symptoms, gait disturbances are also characteristic, caused by weakness, soreness of movements, stiffness of the joints. A compression fracture is a very serious injury and requires treatment and rehabilitation.
Vertebral instability
Vertebral instability is another cause of gait disorders. This condition can be caused by back injuries, for example, when it is overextended, unsuccessfully landing after a jump. In case of instability, the vertebrae “lose” their connection with each other, slide relative to each other, squeezing the nerve roots and blood vessels, causing pain and stiffness of movements. Often the pain radiates to the legs, especially if the pathological process is localized in the lumbar spine, which affects the gait.
In general, pain in the spine leads to stiff, slow walking in small steps, lumbar lordosis decreases. Patients usually seek to reduce heel strike at the very beginning of the stance phase.
Damage to the lower limbs
Coxalgic gait
Coxalgic gait is typical for patients with affected hip joint. The cause of such a disorder may be trauma, damage to the joint, ligamentous apparatus. When walking, patients shift the upper half of the body towards the injury during the stance phase on the affected leg. This gait adapts the patient to injury, reduces the impact on the affected hip during the stance phase.
Antalgic gait
Antalgic gait is typical for of knee joint injuries, ankle sprains, and stress fractures of the foot. In order to avoid pain, the patient minimally uses the affected limb for support, which leads to lameness. To further reduce stress on the affected side, patients raise and lower the leg with a fixed ankle position. In order to alleviate the patient’s condition, at first crutches or other accessories are used to transfer support from the lower limb to the upper ones.
Gait with hyperextension of the knee joint
Hyperextension of the knee joint is associated with an injury in which the joint is blown anteriorly. Such an injury often causes a tear in the anterior cruciate ligament of the knee (ACL). A patient cannot lean on the leg, the knee swells strongly, symptoms of a “pseudo-block” appear – the impossibility of flexion and extension in the knee joint. The knee is held by posterior ligaments. Increasing the angle of leg flexion at the ankle joint, as well as extension of the hip, serves to extend and transfer the affected leg during the stance phase.
Video: “Post-traumatic rehabilitation of gait disorders“
EXERCISES FOR POST-TRAUMATIC CORRECTION AND REHABILITATION OF GAIT. INITIAL STAGE – SET 1
For additional information about Post-traumatic rehabilitation of gait disorders you can watch a video demonstrating exercises and rehabilitation recommendations.
Treatment and correction of gait disorders
The first and most important step in the correction of gait disorders is to eliminate the cause of the disorder. In the event of an injury, it is necessary to contact a medical specialist and undergo a thorough examination. If damage to the nervous system is found, such as the spinal cord, brain or peripheral nerves, complex treatment will be indicated to a patient will by a dedicated specialist, depending on the nature of the damage.
If the injury has caused damage to the musculoskeletal system: ligament ruptures, joint damage, fractures – during the acute phase, rest and adherence to the regimen is indicated to a patient, drug therapy is prescribed, more often analgesics and anti-inflammatory drugs. If necessary, surgical treatment of the injury is indicated. Further rehabilitation of the patient is indicated by a physiotherapist or rehabilitation specialist under the supervision of the attending physician. A properly selected rehabilitation program allows you to restore lost functions and correct gait disorders.

Mandatory chains of rehabilitation therapy
Therapeutic exercise
A set of exercises selected for a patient allows you to strengthen the musculoskeletal system, restore balance and body sensation in space, develop affected joints and ligaments. Common exercises, such as those aimed at increasing muscle strength and resistance, as well as balance training, can increase habitual and maximum rate and quality of walking.
Mechanotherapy
Activity on special simulators is carried out in an individual mode, with a gradual increase in load and is indicated for a smooth return to physiological movements. The purpose of the exercises is the maximum possible restoration of the function of the limbs, the development of new motor stereotypes.
Massage
It is an additional method of rehabilitation, improves blood circulation, develops muscles, eliminates pain and discomfort.
An individual program of physiotherapy
An individual program of physiotherapy methods is selected, including thermal procedures, electrical stimulation. The methods are aimed at improving the blood supply and functioning of the muscles and joints of the affected area, reducing pain and inflammation.
orthopedic interventions
In rare cases, patients need orthopedic interventions to eliminate secondary disorders of the musculoskeletal system. It is possible to move muscles and tendons, eliminate joint contractures, etc.

what gait correction prevents
Post-traumatic rehabilitation allows a patient to get rid of gait disorders or weaken the manifestations of a pathological stereotype during gait.
Adequate gait correction can prevent:
-
painful sensations;
-
disruption of daily functioning;
-
repeated injuries and bruises;
-
loss of motor ability;
-
deformation of the musculoskeletal system.
-
development of a compensatory, incorrect walking stereotype.

CHECK OUT THE DEMO VERSION OF OUR EXERCISES FOR Post-traumatic rehabilitation of gait disorders ON YOUTUBE.
Our website presents the following sets of exercises for Post-traumatic rehabilitation of gait disorders:
-
EXERCISES FOR POST-TRAUMATIC CORRECTION AND REHABILITATION OF GAIT. INITIAL STAGE – SET 1
-
EXERCISES FOR POST-TRAUMATIC CORRECTION AND REHABILITATION OF GAIT. MIDDLE STAGE – SET 2
-
EXERCISES FOR POST-TRAUMATIC CORRECTION AND REHABILITATION OF GAIT. ADVANCED STAGE – SET 3
-
EXERCISES FOR POST-TRAUMATIC CORRECTION AND REHABILITATION OF GAIT. VERY ADVANCED STAGE – SET 4