Published on December 13, 2022
Medically reviewed by Anita C. Chandrasekaran, MD
While medication is often prescribed to treat osteoporosis, maintaining a healthful diet with the recommended amounts of calcium, vitamin D, protein, and other nutrients is critical to supporting good bone health. Avoiding ultra-processed foods, added sugars, and excess alcohol can also help.
This article looks at the best foods for bone health and foods to avoid to help with osteoporosis.
Video: “EXERCISES FOR THE ELDERLY | SENIOR’S ZONE”
EXERCISES FOR THE ELDERLY/SENIOR’S ZONE. FIRST DIRECTION: REHABILITATION AND SUPPORTIVE THERAPY FOR THE ELDERLY (THERAPEUTIC SET OF EXERCISES). INITIAL STAGE OF REHABILITATION
For additional information about exercises for the elderly | Senior’s zone you can watch a video demonstrating exercises and rehabilitation recommendations.
Benefits
A balanced diet that includes nutrients such as calcium, vitamin D, and protein, helps prevent further bone loss and reduces the risk of fractures. This eating pattern can also help prevent osteoporosis in those without the condition.1
Calcium
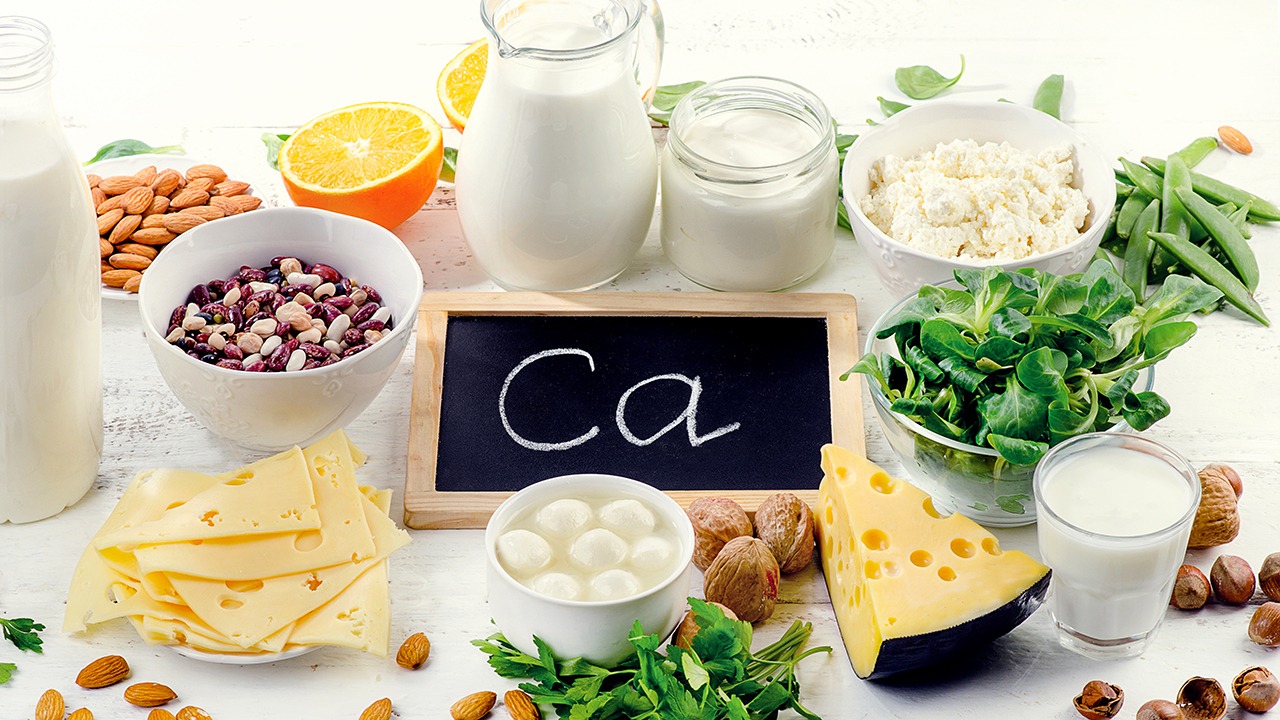
Calcium is vital for building and maintaining strong bones. Inadequate calcium intake throughout life is associated with low bone density and high fracture rates.2 When you don’t consume enough calcium in your diet, your body pulls calcium from your bones, which can contribute to bone loss.3
Though some individuals require a calcium supplement, they should be used with caution and under the supervision of a healthcare provider. Studies have linked calcium supplements to an increased risk of kidney stones, colon polyps (small growths in the large intestine), and heart disease.45
Foods high in calcium include:6
- Milk
- Cheese
- Yogurt
- Dark, leafy green vegetables, such as kale, spinach, and collard greens
- Tofu
- Nuts and seeds
- Legumes
- Canned salmon and sardines with bones
Daily Recommended Calcium Intake
Females who are 51 years and older require 1,200 milligrams of calcium daily, while males need 1,000 milligrams. Beginning at age 70, men and women require 1,200 milligrams daily.2
Vitamin D
Your body needs vitamin D to absorb calcium and keep muscles strong. Low vitamin D levels are associated with decreased bone density, which can lead to osteoporosis and broken bones.78

You can get vitamin D from the sunlight and from eating vitamin D–rich foods. However, few foods are naturally rich in vitamin D. The best sources are the flesh of oily fish such as trout, salmon, or tuna and fish liver oils.9
Other dietary sources of vitamin D include:
- Orange juice fortified with vitamin D
- Beef liver
- Mushrooms
- Egg yolks
- Sardines
- Plant-based milk fortified with vitamin D
- Cheddar cheese
Daily Recommended Vitamin D Intake
Individuals 70 and younger should consume 600 IU (international units) of vitamin D daily. People over 70 should increase their consumption to 800 IU daily.2
Protein
Around 50% of your total bone volume and about one-third of bone mass is made of proteins. Dietary protein affects the secretion and action of insulin-like growth factor I (IGF-I), a hormone essential for bone formation.10

While it was once believed that too much protein might cause a negative calcium balance and bone loss, some studies suggest that a protein-rich diet, combined with adequate dietary calcium intake, is essential for bone health.10
Good dietary sources of protein include:
- Lean meat
- Seafood
- Eggs
- Beans
- Legumes
- Nuts and seeds
How Much Protein Do I Need?
Many experts recommend a dietary protein intake of 1.0–1.2 grams per kilogram of body weight per day, including around 20–25 grams of high-quality protein at each meal.10
Other Nutrients
Dietary patterns rich in fruit and vegetables are associated with higher bone mineral density.11
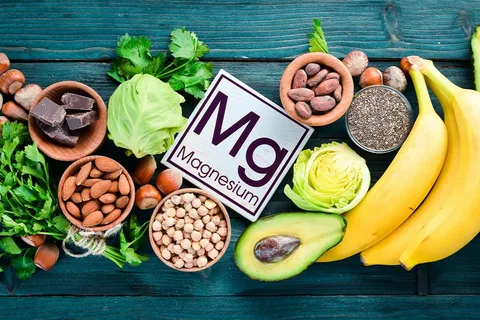
Vitamins and minerals commonly found in fruits and vegetables that play a role in bone health include:11
-
Magnesium
-
Potassium
-
Vitamin K
-
Vitamin C
-
Carotenoids
How It Works
A good diet for osteoporosis incorporates various nutrients that support bone health. There are no special rules, but try to eat more nutrient-dense foods to ensure optimal amounts of vitamins, minerals, protein, and other vital nutrients daily.
Studies suggest that a calcium intake that meets the current recommended daily allowance and a Mediterranean-style diet may be effective in maintaining good bone health and preventing osteoporosis.12
High intakes of fruits, vegetables, legumes, nuts, whole grains, fish, seafood, and extra virgin olive oil are included in the Mediterranean diet. It is generally low in red meat.13
What If I Am Lactose Intolerant or Follow a Vegan Diet?
Eating dark, leafy greens, colorful veggies, beans, and nuts, as well as spending a moderate amount of time in the sunshine, are good ways to meet your daily protein, calcium, and vitamin D requirements without dairy or meat products.
Foods to Avoid, Limit, or Replace
The overconsumption of certain foods, such as added sugar, salt, ultra-processed foods, caffeine, and alcohol, may lead to bone loss and increase your risk for osteoporosis.
Ultra-Processed Foods
One study found that diets rich in red and processed meat, refined grains, and sweets were linked to a lower bone mineral density and a higher fracture risk.10
Another study linked diets high in ultra-processed foods, such as cheese, french fries, processed meat, pastries, pizza, snacks, and refined grains, with a lower bone mineral density when compared to other diets.11
A high fat intake mainly derived from processed foods directly interferes with calcium absorption in the gut. It also places you at a greater risk for obesity, which can also negatively affect bone health.10 Replacing high-fat processed foods with healthy fats, such as avocado and olive oil, can also help you maintain a healthy weight.
Salt and Sugar
Too much salt may increase the amount of calcium your body excretes with urination. Aim to consume less than 2,300 milligrams per day, equal to about 1 teaspoon of table salt.2
Overconsumption of added sugars may increase the risk of osteoporosis by reducing calcium absorption in the gut, increasing the urinary excretion of calcium and magnesium, and impairing bone formation.14
Reduce your salt intake by swapping prepackaged snacks for whole foods, chicken broth for low-sodium chicken broth, and processed meats for fresh proteins flavored with herbs and spices. Moreover, many sodas are high in sugar and phosphoric acid additives, which can prevent bone mineralization.
Caffeine
Caffeine may interfere with calcium absorption. However, evidence to support its effects on bone health remains limited.
One study found that the consumption of 800 milligrams of caffeine resulted in a 77% increase in calcium eliminated by the kidneys compared to a placebo (a substance containing no caffeine) over nine hours.15 Another study found that people who regularly drank coffee had higher bone mineral density than non-coffee drinkers.16
If you’re a coffee drinker, aim for two to three cups daily, as long as you eat enough calcium-rich foods.17 One 8 ounce cup of coffee has around 96 grams of caffeine. Swap caffeinated beverages for flavored water or decaffeinated coffee or tea to reduce caffeine intake.
Alcohol
Excessive alcohol consumption interferes with calcium balance, and the body’s natural production of vitamin D.18 Individuals with alcoholism also tend to have high levels of cortisol, which can increase bone breakdown and decrease bone formation.
Excess drinking can cause hormone deficiencies in both men and women. Males may produce lower amounts of testosterone, a hormone linked to bone formation. Females may experience irregular menstrual cycles, which can reduce estrogen levels and increase the risk of osteoporosis.
Summary

A balanced diet rich in bone-supporting nutrients like protein, calcium, and vitamin D and low in ultra-processed foods, alcohol, added sugar, and sodium is best to support bone health. You may also want to limit your daily caffeine intake. If you’d like to develop an osteoporosis meal plan tailored to your health needs and dietary preferences, consider working with a registered dietitian.
By Lindsey DeSoto, RD, LD
Lindsey Desoto is a registered dietitian with experience working with clients to improve their diet for health-related reasons. She enjoys staying up to date on the latest research and translating nutrition science into practical eating advice to help others live healthier lives.
Conclusion
Osteoporosis is a common condition that can be treated with healthy lifestyle habits and, sometimes, medications. Many people can achieve healthy calcium and vitamin D levels by following a balanced, nutrient-dense diet, while others may still require supplementation. Work closely with your healthcare provider to determine the best osteoporosis treatment plan for you.
FREQUENTLY ASKED QUESTIONS
Do certain foods make osteoporosis worse?
Foods with a lot of added sugar and salt, such as processed foods, can increase the amount of calcium your body loses through urination. Excessive alcohol consumption can also interfere with the balance of calcium in the body and vitamin D production.
Does diet directly affect osteoporosis?
Yes. A diet chronically low in calcium and vitamin D is associated with low bone density, which can contribute to the development of osteoporosis.
What are other natural ways to increase body density?
In addition to eating a healthy diet, performing weight-bearing and resistance exercises can help you improve bone health.

DEMO VERSION OF GHRS WORKOUTS FOR THE REABILITAITON OF the elderly | Senior’s Zone ON YOUTUBE
Our website presents sets of exercises for the rehabilitation of the elderly | Senior’s Zone in the following areas:
-
EXERCISES FOR THE ELDERLY/SENIOR’S ZONE. FIRST DIRECTION: REHABILITATION AND SUPPORTIVE THERAPY FOR THE ELDERLY (THERAPEUTIC SET OF EXERCISES). INITIAL STAGE OF REHABILITATION
-
EXERCISES FOR THE ELDERLY/SENIOR’S ZONE. FIRST DIRECTION: REHABILITATION AND SUPPORTIVE THERAPY FOR THE ELDERLY (THERAPEUTIC SET OF EXERCISES). MIDDLE STAGE OF REHABILITATION
-
EXERCISES FOR THE ELDERLY/SENIOR’S ZONE. FIRST DIRECTION: REHABILITATION AND SUPPORTIVE THERAPY FOR THE ELDERLY (THERAPEUTIC SET OF EXERCISES). ADVANCED STAGE OF REHABILITATION
-
EXERCISES FOR THE ELDERLY/SENIOR’S ZONE. SECOND DIRECTION: IMPROVEMENT OF EQUILIBRIUM AND BALANCE, PREVENTION OF FALLS. INITIAL STAGE OF REHABILITATION
-
EXERCISES FOR THE ELDERLY/SENIOR’S ZONE. SECOND DIRECTION: IMPROVEMENT OF EQUILIBRIUM AND BALANCE, PREVENTION OF FALLS. ADVANCED STAGE OF REHABILITATION
Sources
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. Osteoporosis: Diagnosis, treatment, and steps to take.
- National Institutes of Health Osteoporosis and Related Bone Diseases National Resource Center. Calcium and vitamin D: Important at every age.
- National Institutes of Health Osteoporosis and Related Bone Diseases National Resource Center. Osteoporosis overview.
- Johns Hopkins Medicine. Calcium supplements: Should you take them?
- Park JM, Lee B, Kim YS, et al. Calcium supplementation, risk of cardiovascular diseases, and mortality: a real-world study of the korean national health insurance service data. Nutrients. 2022;14(12):2538. doi:https://doi.org/10.3390/nu14122538
- Dietary Guidelines for Americans. Food sources of calcium.
- MedlinePlus. Vitamin D deficiency.
- International Osteoporosis Foundation. Vitamin D.
- National Institutes of Health. Vitamin D.
- Muñoz-Garach A, García-Fontana B, Muñoz-Torres M. Nutrients and dietary patterns related to osteoporosis. Nutrients. 2020;12(7):1986. doi:10.3390/nu12071986
- Sahni S, Mangano KM, McLean RR, Hannan MT, Kiel DP. Dietary approaches for bone health: lessons from the framingham osteoporosis study. Curr Osteoporos Rep. 2015;13(4):245-255. doi:10.1007/s11914-015-0272-1
- Quattrini S, Pampaloni B, Gronchi G, Giusti F, Brandi ML. The mediterranean diet in osteoporosis prevention: an insight in a peri- and post-menopausal population. Nutrients. 2021;13(2):531. doi:10.3390/nu13020531
- Schwingshackl L, Morze J, Hoffmann G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br J Pharmacol. 2020;177(6):1241-1257. doi:10.1111/bph.14778
- DiNicolantonio JJ, Mehta V, Zaman SB, O’Keefe JH. Not salt but sugar as aetiological in osteoporosis: a review. Mo Med. 2018;115(3):247-252.
- Reuter SE, Schultz HB, Ward MB, et al. The effect of high-dose, short-term caffeine intake on the renal clearance of calcium, sodium and creatinine in healthy adults. Br J Clin Pharmacol. 2021;87(11):4461-4466. doi:10.1111/bcp.14856
- Chau YP, Au PCM, Li GHY, et al. Serum metabolome of coffee consumption and its association with bone mineral density: the hong kong osteoporosis study. The Journal of Clinical Endocrinology & Metabolism. 2020;105(3):e619-e627. doi:10.1210/clinem/dgz210
- Kim SY. Coffee consumption and risk of osteoporosis. Korean J Fam Med. 2014;35(1):1. doi:https://doi.org/10.4082/kjfm.2014.35.1.1
- National Institutes of Health Osteoporosis and Related Bone Diseases National Resource Center. What people recovering from alcoholism need to know about osteoporosis.








