The recovery process following a patellar fracture requires time, patience, and the correct rehabilitation approach. From comprehensive diagnosis to a gradual return to normal life, each stage of the rehabilitation process is crucial. Watch the video exercises for patellar fracture rehabilitation for additional information and support.

When can you start home rehabilitation with our exercises?
A kneecap fracture can significantly affect your mobility and quality of life. Our subscription offers you valuable resources for effective and safe home rehabilitation, with exercises designed in collaboration with Israeli specialists.
It is important to begin rehabilitation at the right time to expedite recovery:
- Acute Phase: It is essential for initial pain and inflammation to relieve. This may take several weeks after the injury.
- Medical Approval: Be sure to obtain permission from your treating physician or orthopedist before starting home exercises.
What is Included in the Subscription?
- Video Instructions: Our detailed video guides demonstrate how to perform correctly each exercise, which is crucial to prevent further injuries.
- Written Instructions and Infographics: You will also have access to written instructions and visual infographics for better comprehension and execution of exercises.
- Repetition Guidelines: We provide clear instructions on the number and intensity of repetitions to ensure a safe increase in workload.
Benefits of Home Rehabilitation
- Convenience and Control: Perform exercises at your convenience, controlling your recovery pace.
- Personalized Approach: Our program considers individual characteristics and recovery stages of each patient.
- Continuous Access to Materials: At any time, you can revisit videos and instructions for repetition or clarification of the exercise sequence.
- Comfortable Support: It is easier to create a favorable and calm atmosphere for rehabilitation in the comfort of your home.
Try our subscription for good-quality and comfortable rehabilitation after a kneecap fracture!
Watch Video Exercises for Rehabilitation After Kneecap Fracture
Video: “exercises for Rehabilitation of the Knee Joint”
Exercises for the knee joint. Set 4A is aimed at strengthening the muscles. Initial stage.
For additional information about postoperative rehabilitation of the knee joint you can watch a video demonstrating exercises and rehabilitation recommendations.
How to Recognize a Patellar Fracture
Understanding the signs and symptoms of a patellar fracture is crucial for seeking timely medical care and preventing further complications. Here are key aspects to pay attention to:

Typical Symptoms of a Patellar Fracture
- Sharp Pain: One of the first and most acute signs of a patellar fracture is sharp pain around the knee, especially when attempting to move or put weight on the leg.
- Swelling and Redness: A patellar fracture is accompanied by swelling, redness, and sometimes an increase in skin temperature around the injured area.
- Bruising and Discoloration: Bruises and hematomas may appear due to damage to blood vessels during the injury.
- Limited Mobility: The injured knee often loses its normal range of motion, and the patient may have difficulty bending or straightening the leg.
External Signs and Sensations
- Knee Deformation: In some cases, a patellar fracture can lead to noticeable deformation in the knee joint area.
- Feeling of Cracking or Popping: Patients sometimes describe a sensation of cracking or popping at the moment of injury.
- Inability to Bear Weight: In severe cases of patellar fracture, a person may not be able to stand or bear weight on the affected leg.
The Need for Immediate Medical Care
If you suspect a patellar fracture, it is essential to seek medical care as soon as possible. Before the arrival of ambulance team, try to keep the injured limb at rest, apply cold to the site of the injury to reduce swelling, and, if possible, elevate the injured leg. Delaying medical care can increase the risk of complications and prolong the recovery period.
In the presence of these signs, it is important not to attempt to self-treat and avoid additional load on the injured knee to prevent worsening the injury.
Basics of a Patellar Fracture
A patellar fracture is a serious injury that requires careful treatment and rehabilitation. Understanding the fundamentals of this injury can help optimize the recovery process.

What Is a Patellar Fracture?
A patellar fracture involves damage to the kneecap, a small, round bone that protects the knee joint. This bone plays a crucial role in the mechanism of flexion and extension movements of the knee, as well as in stabilizing and distributing loads on the knee joint.
Causes and Risk Factors
Patellar fractures most commonly occur as a result of a direct blow to the knee, such as falling on the knees or car accidents. Risk factors include engaging in certain sports (e.g., skiing or football), osteoporosis, and pre-existing knee conditions that weaken the bone.
Consequences of a Patellar Fracture
The consequences of a patellar fracture can vary from temporary mobility limitations and pain to long-term problems with the knee joint, such as arthritis, chronic pain, and reduced joint function. In severe cases, surgical intervention may be required to restore the structure and function of the kneecap.
Classification of Patellar Fractures
Patellar fractures can vary in severity and the nature of the damage. The classification of fractures helps determine an appropriate treatment and rehabilitation strategy. Below are the main types of patellar fractures.
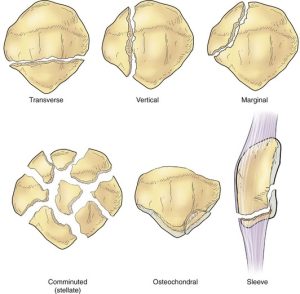
Marginal Fractures
- Description: A marginal fracture occurs when a small fragment of bone at the edge of the patella is detached. This type of fracture is often a results of a direct blow or a fall onto the knee.
- Treatment: Most marginal fractures can be treated conservatively, using a plaster cast or brace to immobilize and protect the knee during the healing process.
Longitudinal Fractures
- Description: Longitudinal fractures occur along the length of the patella. They can be stable (without displacement) or unstable (with displacement of bone fragments).
- Treatment: Stable longitudinal fractures are often treated conservatively. Unstable fractures, especially with a significant displacement, may require surgical intervention to restore the anatomy of the patella.
Transverse Fractures
- Description: A transverse fracture occurs horizontally across the patella. These fractures are often related to ligament damage, increasing the risk of knee instability.
- Treatment: Transverse fractures, especially with significant displacement, typically require surgical intervention using screws, wires, or other fixation devices to restore and stabilize the patellar structure.
Comminuted Fractures
- Description: A comminuted fracture is characterized by the patella shattering into multiple pieces. This type of fracture is one of the most complex and often occurs due to high-energy trauma.
- Treatment: Treating comminuted fractures usually involves surgical intervention to restore the shape and functionality of the patella. In some cases, reconstruction or even replacement of the patella may be necessary.
Understanding the type of patellar fracture helps doctors develop the most effective treatment and rehabilitation plan, aiming to for maximum restoration of knee joint function and a reduced risk of future complications.
Initial Steps After Injury
Taking the right steps immediately after a patellar injury is crucial to ensure effective recovery and minimize the risk of complications. Here are the key points to consider immediately after being injured.

Medical Care and Diagnosis
- Immediate Medical Attention: When there is suspicion of a patellar fracture, it is crucial to seek medical care as soon as possible. Consult a physician or visit the nearest emergency department.
- Diagnostic Procedures: In most cases, an X-ray is performed to confirm the diagnosis. In some cases, additional diagnostics such as computed tomography (CT) or magnetic resonance imaging (MRI) may be required to assess the extent of damage to bone and soft tissues.
Examinations/Tests at MRI Clinics
MRI clinics offer high-precision imaging methods that help doctors get a more comprehensive presentation of the injury. This can be especially important in cases of complex or unusual fractures.
Surgical Intervention and Immobilization
- Assessment of the Need for Surgical Intervention: Depending on the type and severity of the fracture, surgery may be required to restore and stabilize the patella.
- Immobilization: Immobilization with the use of a plaster cast, brace, or special splint is often applied to protect the injured area and provide conditions for healing.
Planning Further Treatment and Rehabilitation
- Development of a Treatment Plan: After assessing the injury, the physician will develop an individualized treatment plan, which may include both conservative and surgical treatment methods.
- Preparation for Rehabilitation: The initiation of rehabilitation measures is typically planned already at the stage of initial medical care stage to ensure the best conditions for recovery.
The initial steps after the injury form the foundation for successful treatment and recovery after a patellar fracture. Timely and adequate medical intervention helps reduce the risk of complications and accelerates the recovery process.
Rehabilitation Process
Rehabilitation after a patellar fracture is a key stage in restoring functionality and mobility of the knee joint. This process includes several stages and methods aimed at a gradual return to normal life and activities.

Rehabilitation Stages
- Acute Stage: This stage begins immediately after the injury or surgery. The primary goal at this stage is to reduce pain and swelling while preventing complications. Maintaining the range of motion in the joint to the extent possible is an important element.
- Subacute Stage: During this stage, the focus shifts towards regaining mobility, strengthening muscles, and improving coordination. Exercises become more active and are aimed at enhancing knee function.
- Late Stage: The final stage of rehabilitation is focused on returning to regular daily and professional activities. It includes exercises for strengthening, balance, and adaptation to more complex tasks.
Importance of Early Mobilization
Early mobilization is critically important for preventing joint stiffness and muscle atrophy. Initial restoration of motor activity contributes to improved blood circulation and accelerates the healing process.
Rehabilitation Methods
Various methods are used in the rehabilitation after a patellar fracture to expedite recovery and return to normal life.

Physiotherapy
Physiotherapy plays a central role in the rehabilitation process and includes a variety of procedures and techniques:
- Electrotherapy: Using electrical currents to reduce pain and stimulate muscle activity.
- Ultrasound Therapy: Application of ultrasound waves to improve blood circulation and accelerate the healing process.
- Cryotherapy (Cold Therapy): Reducing swelling and pain by applying cold to the injured area.
- Heat Therapies: Using heat to relax muscles and improve blood circulation.
- Manual Therapy: This includes massage, stretching, and joint mobilization to enhance mobility and reduce pain.
List of 20 Exercises for Strengthening and Recovery After a Patellar Fracture

Early Stage
- Toe Flexing and Extending: Promotes improved blood circulation.
- Quadriceps Contractions: Tightening the muscles at the front of the thigh while holding the tension.
- Straight Leg Raises While Lying Down: Lift the leg while keeping it straight.
- Ankle Rotations: Rotate the ankle in both directions to enhance mobility.
- Hip Raises While Lying Down: Lift the hip while keeping the leg straight.
Subacute Stage
- Knee Bends with Elastic Band: Use a resistance band to bend the knee.
- Gentle Chair Squats: Perform squats while holding onto a chair or table for support.
- Gentle Ball Exercises: Roll a ball with your feet while sitting in a chair.
- High Knee Marching: March in place while lifting your knees.
- Standing Calf Raises: Strengthen calf muscles.
Late Stage
- Step-Ups: Step onto a step or platform with one leg, then the other.
- Sideways Steps with a Resistance Band: Take sideways steps with a band around your thighs.
- Lying Down Bicycle Kicks: Simulate riding a bicycle while lying on your back.
- Squats with a Ball Against the Wall: Squat with back support from a wall and a ball behind your back.
- Step Back with Knee Raise: Step backward and then raise your knee.
Exercises to Improve Balance and Coordination
- One-Legged Stand: Improve balance and stability by standing on one leg.
- Yoga or Pilates: Exercises to strengthen muscles and enhance flexibility.
- Dance Therapy: Enhance coordination and balance through dance exercises.
- Use of a Balance Board: Balance board exercises to improve knee stability.
- Walking on a Straight Line: Similar to a sobriety test, this improves coordination and balance.
Each exercise should be performed considering the patient’s individual characteristics and under the guidance of a qualified specialist to ensure safety and effectiveness.
Diet and Lifestyle During Rehabilitation
Diet and lifestyle play a crucial role in the recovery process after a patellar fracture. Adequate diet provides the body with essential nutrients for bone healing and muscle recovery, while a healthy lifestyle promotes general well-being and accelerates the healing process.
The Role of Balanced Nutrition
- Bone Tissue Recovery: Consuming foods rich in calcium (dairy products, green leafy vegetables, broccoli) and vitamin D (fish, egg yolks, moderate sun exposure) is important for fracture healing and bone strength.
- Protein for Muscle Strength: Adequate protein intake is crucial for muscle recovery. Sources of protein include meat, fish, legumes, nuts, and seeds.
- Vitamins and Minerals: Fruits and vegetables provide vitamins and minerals that contribute to the overall recovery process and support the immune system.
The Importance of Sufficient Rest and Sleep
- Significance of Sleep: Quality sleep is critical for the body’s recovery processes. During the sleep, the production of growth hormones increases, which contributes to tissue healing.
- Regular Rest: Periods of rest throughout the day help reduce fatigue and prevent overloading the injured leg.
Lifestyle Modification
- Moderate Physical Activity: Regular light exercises that align with the rehabilitation plan help maintain blood circulation and general
- Avoiding Harmful Habits: Smoking and excessive alcohol consumption can slow down the healing and recovery process, so it is recommended to limit or completely eliminate these habits.
- Emotional Well-being: Managing stress and maintaining a positive mood are also important for successful recovery. Relaxation techniques, meditation, or consultations with a psychotherapist can be helpful in this process.
Integrating healthy diet and lifestyle into the rehabilitation plan improves general health and contributes to a faster and more effective recovery after a patellar fracture.
Psychological Support
Psychological support is an essential part of the rehabilitation process after a patellar fracture. It helps patients cope with the emotional and psychological challenges associated with the injury and subsequent recovery. Here are some practical aspects in which psychological support can be expressed:

Coping with Stress and Anxiety
- Individual Counseling: A psychotherapist can help the patient understand his feelings related to the injury and the recovery process.
- Relaxation Techniques: Training relaxation techniques such as breathing exercises, meditation, or yoga to reduce stress and anxiety.
Why Psychological Support Matters
- Enhancing Motivation: Psychological support helps improve the patient’s motivation for rehabilitation by setting realistic goals and plans for achievement.
- Dealing with Lifestyle Changes: Adapting to temporary activity limitations and lifestyle changes can be emotionally challenging. A psychologist helps the patient develop strategies for adapting to new conditions.
- Rebuilding Confidence: Working on recovering self-esteem and confidence in one’s physical abilities after an injury.
Group Therapy and Support Groups
- Sharing Experiences with Fellow Patients: Participating in group sessions or support groups allows individuals to exchange experiences and get support from others going through similar difficulties.
- Family Therapy: Sometimes, involving family members can be beneficial, so they better understand how to support the patient in the recovery process.
Psychological support helps ensure a more comprehensive and effective approach to rehabilitation, taking into account not only the physical but also the emotional aspects of recovery. It is important that such support is available and integrated into the entire rehabilitation plan.

Frequently asked Questions
Question 1: Is it necessary to wear a brace or orthosis after a kneecap fracture?
Answer: Yes, often doctors recommend wearing a brace or orthosis after a kneecap fracture to provide support and stability to the joint during the healing process and initial stages of rehabilitation. This helps prevent additional injuries and promotes proper recovery.
Question 2: Is it possible to regain fully knee function after a kneecap fracture?
Answer: In most cases, it is possible to achieve full knee function recovery after a kneecap fracture, especially with timely and adequate treatment and rehabilitation. However, the rate and degree of recovery may vary depending on the complexity of the fracture and the individual characteristics of the patient.
Question 3: What types of sports are recommended after recovering from a kneecap fracture?
Answer: After a full recovery from a kneecap fracture, low-impact sports such as swimming, cycling, Pilates, and walking are recommended. These activities help strengthen muscles and joints without excessive strain.
Question 4: Can swimming expedite the rehabilitation process?
Answer: Yes, swimming is an excellent method of rehabilitation as it helps strengthen muscles without putting excessive pressure on the joints. The water provides natural resistance, which contributes to improved strength and flexibility.









