A tibial fracture is a common injury that can significantly affect a person’s daily life and mobility.
Lack of appropriate medical intervention and insufficient rehabilitation can lead to chronic problems and complications, such as deformity and chronic pain.
Effective rehabilitation after a tibial fracture can noticeably accelerate the recovery process and minimize the risks of complications. This article will cover the key stages of the rehabilitation process, including physiotherapy, diet and psychological support.
Now that we’ve identified the primary problem and offered a solution, let’s delve into how to effectively approach rehabilitation after a tibial fracture at different stages of recovery.
Key Concepts and Definitions

What Is the Tibia and Its Functions
The tibia, also known as the shinbone, is one of the two bones that make up the lower leg and plays a crucial role in providing stability and mobility to the leg. Its counterpart is the fibula.
Types of Tibial Fractures
Tibial fractures can be closed or open, displaced or non-displaced, ranging from simple ones that don’t require surgical intervention to complex ones involving damage to the bone tissue. Depending on the degree of damage, fractures are categorized into several types: linear, spiral, comminuted, etc.
Linear Fractures
Linear fractures are characterized by a straight-line break in the bone tissue that doesn’t result in fragment displacement. Typically considered relatively “favorable”, these fractures don’t involve significant bone destruction and tend to heal quickly. Nevertheless, even seemingly simple linear fractures require a competent approach to rehabilitation to avoid long-term consequences.
Spiral Fractures
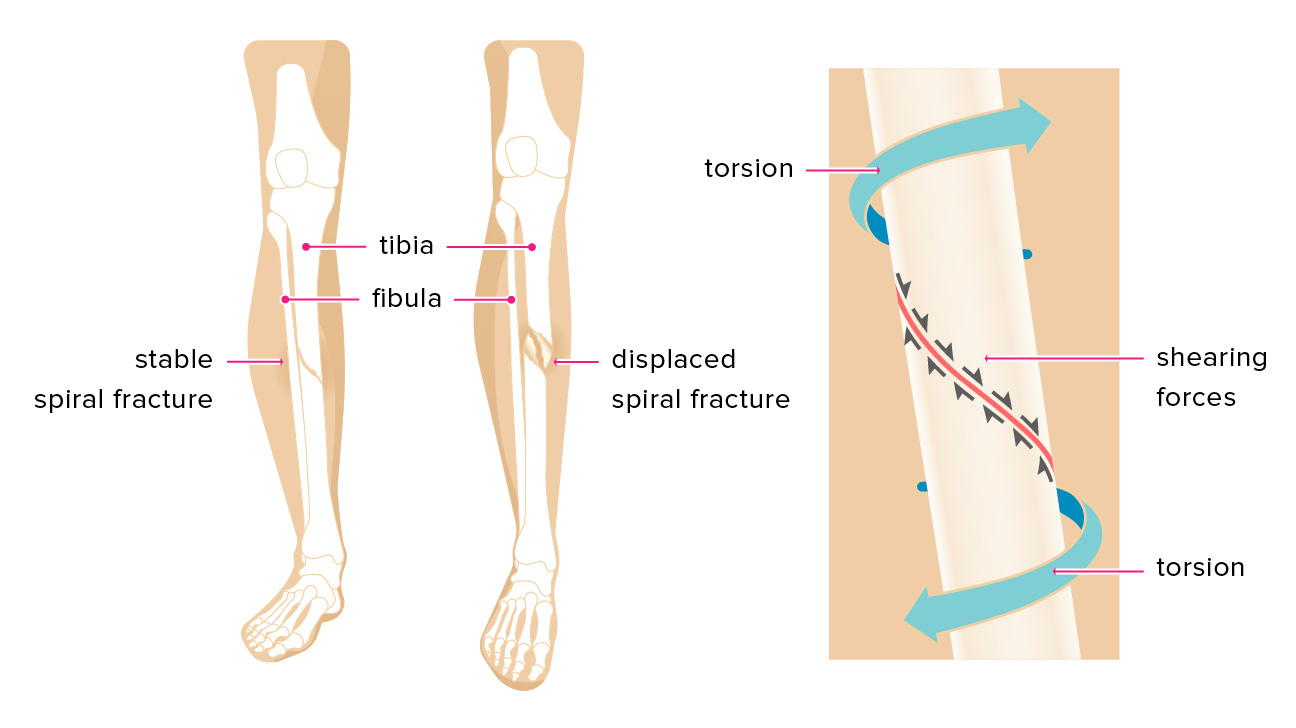
Spiral fractures occur due to twisting of the limb and are characterized by a “spiraling” pattern of bone tissue rupture. These fractures often lead to fragment displacement and usually require surgical intervention to stabilize and adequately restore the tibia or fibula. Spiral fractures can be particularly challenging in rehabilitation, as they often involve damage to soft tissues surrounding the bone.
Both types of fractures require an individualized approach when selecting a treatment method and rehabilitation plan.
Symptoms and Diagnosis

Pain Syndrome
One of the most prominent symptoms of a fracture is pain. Patients often describe acute, piercing pain at the site of the fracture. The intensity of the pain can vary depending on the type of fracture, but even minor fractures typically come with significant discomfort. Pain worsens when attempting to move the affected limb and may persist even at complete rest.
Fractures with Displacement
Fractures with displacement of bone fragments, such as spiral or comminuted fractures of the tibia or fibula, pose a particular challenge. They often involve damage to the surrounding soft tissues and tendons. In cases of displaced fractures, it is crucial to seek medical attention promptly to stabilize the position of bone fragments and prevent further complications.
Swelling, Hematomas, and Visible Deformities
In addition to pain, swelling, hematomas, or even visible limb deformity are often observed at the site of the fracture. These symptoms require immediate diagnosis and treatment. Modern diagnostic methods, such as X-rays or MRI scans, enable a high-precision assessment of the nature of the fracture and its complexity, which is a crucial factor in selecting the treatment method and rehabilitation plan.
Understanding the basic symptoms and diagnostic methods for fractures of the tibia and fibula, as well as bone tissue in general, is the first step towards effective rehabilitation after a tibial fracture. This helps doctors and patients collaboratively develop the most effective treatment and rehabilitation plan.
Treatment Methods and Initial Rehabilitation Steps

Surgical Treatment
Treatment and rehabilitation after a tibial fracture, including the fibula, depend on various factors: the type of fracture, the presence of displacement, the patient’s general condition, etc. Below, we will discuss the primary treatment methods and initial steps in the rehabilitation process.
Osteosynthesis

Osteosynthesis is a surgical method of fixing fractured bone fragments to accelerate their healing and restore limb function. The procedure involves the application of metal plates, pins, or screws, which serve as a “skeleton” to stabilize the fracture. It is widely used in orthopedic surgery and can be performed through open or closed methods.
Open and Closed Methods
In the open method, a surgeon makes an incision above the fracture site and directly fixes the bone fragments. This allows for a clear view of the fracture and precise placement of the fixation elements. The closed method involves minimal surgical incisions and the use of X-ray control to install metal elements. It is preferred to minimize the risk of infections and \accelerate the healing process.
Selection of Material
Materials for osteosynthesis can vary, including titanium, stainless steel, and cobalt alloys. The selection depends on several factors, including the possibility of allergic reactions, cost, and durability.
Advantages and Disadvantages
Advantages of osteosynthesis include rapid bone healing and restoration of limb function, the ability to load the limb early, and a reduced risk of deformities. However, the method has its disadvantages, such as the risk of surgical intervention, the possibility of infection, and additional challenges if a repeated operation is needed.
Metal Osteosynthesis

Metal osteosynthesis is a subset of osteosynthesis that specifies the use of metallic implants to fix fractured bone fragments. This method is widely used in orthopedic surgery to treat various types of fractures, including displaced and comminuted fractures.
Types of Metal Constructions
- Plates and Screws: These are used to fix bone fragments through an open method. Plates are attached to the bone with screws, providing stability at the fracture site.
- Intramedullary Rods: These are inserted into the bone cavity, typically in the case of fractures of long tubular bones, such as the femur or tibia.
- External Fixators: These are used when internal fixation is not possible or undesirable, such as in the presence of infection.
Advantages of Metal Osteosynthesis
- Rate of Recovery: Metallic constructions provide high stability, accelerating the bone fusion process.
- Early Mobilization: In most cases, patients can start moving early in the postoperative period.
- Accuracy of Fixation: The use of metallic constructions allows for precise bone fragment alignment, reducing the risk of deformities and expediting accelerating recovery, e.g., after a small tibial fracture.
Characteristics and Recommendations
- Materials: High-quality metals like titanium are typically used, as they are biocompatible.
- Postoperative Care: Patients may require a course of antibiotics to prevent infections, along with regular medical check-ups to monitor the healing process.
- Implant Removal: In some cases, particularly in successful recoveries, metallic constructions can be removed.
Metal osteosynthesis is currently one of the most effective methods for treating fractures in modern medicine. It offers a high level of reliability and a wide range of applications, making it an integral part of orthopedic practice.
Conservative Treatment
In some cases, especially when fragments are not displaced, surgical intervention may not be necessary. In such cases, a plaster cast or orthopedic devices are used to immobilize the limb.
Selecting a Treatment Method
The selection choice between surgical and conservative methods depends on various factors, including the patient’s age, general health, and the type and complexity of the fracture.
Immobilization and Edema Reduction
The first step after establishing a diagnosis is immobilizing the injured limb. Edema can be reduced using cold compresses and elevating the limb.
Restoration of Blood Circulation and Mobility
The next stage involves restoring blood circulation and mobility with physiotherapy and medications.
Recovery After a Small Tibial Fracture
In the case of a small tibial fracture, the rehabilitation plan may vary. After surgical or conservative treatment, the main focus is on restoring limb function and avoiding complications such as arthritis or inadequate bone fusion.
Video: “Exercises for the Lower Limb Problems“
EXERCISES FOR THE ANKLE JOINT. SET №6E IS AIMED AT STRENGTHENING OF THE MUSCLES AND IMPROVEMENT OF PROPRIOCEPTION AND STABILITY OF THE ANKLE AND ENTIRE LOWER LIMB. MID STAGE
For additional information about the recovery process you can watch a video demonstrating exercises and rehabilitation recommendations.
Rehabilitation Plan: Phases and Timelines

Rehabilitation after a tibia or fibula fracture is a complex and multi-stage process that requires an individualized approach. The main goal is to restore the functionality and structure of affected bones and joints.
Rehabilitation Protocol After Surgery
Following surgical intervention, doctors develop a specialized rehabilitation protocol, often starting with gentle exercises for the joints and soft tissues to improve blood circulation and reduce swelling.
Phase I (0-14 days after surgery)
The first phase of rehabilitation typically lasts from 0 to 14 days and involves immobilization of the limb, along with measures to reduce swelling and pain. Monitoring inflammation levels and checking surgical incisions for possible infection is also important during this phase.
Phase II (2-8 weeks after surgery)
During this stage, exercises to improve muscle strength and coordination begin. Doctors often recommend moderate physical activity as well as procedures to improve blood circulation and reduce swelling.
Phase III (8-16 weeks after surgery)
At this stage, doctors typically allow for the increased load on the limb. Procedures to improve skin and soft tissue elasticity are performed, along with comprehensive balance and coordination exercises.
All these phases require careful medical supervision and regular monitoring to modify the rehabilitation plan in case of complications.
Physiotherapy for Tibia Fractures

Physiotherapy is a the cornerstone of the rehabilitation plan after a tibia or fibula fracture. It not only reduces pain and improves blood circulation but also activates the healing and functional recovery processes of the limb.
Importance of Physiotherapy in Rehabilitation
In practice, physiotherapy begins as early as possible and is performed under the supervision of an experienced physiotherapist. The primary goal is to maximize recovery and minimize the risk of chronic complications, such as muscle atrophy and reduced joint mobility.
Types of Physiotherapy Methods
The following types of physiotherapy are widely used in practice:

- Electrostimulation: Used to alleviate pain and accelerate the regeneration process.
- Ultrasound Therapy: Improves microcirculation and promotes fracture healing.
- Magnetotherapy: Reduces inflammation and swelling at the fracture site.
- Cryotherapy: Used to reduce swelling and pain.
- Heat Therapies: Often used to relax muscles and relieve spasms.
Timelines and Recommendations
Physiotherapy procedures typically begin after the acute phase of pain subsides and are conducted performed 3-5 times per week. The duration of the course depends on the extent of the injury and can range from 2 to 8 weeks.
Examples of Exercises for Recovery After a Tibia Fracture
After being allowed/approved by a doctor and a physiotherapist, these exercises can be included in your rehabilitation plan to accelerate the recovery process. Keep in mind that each case is unique, and some exercises may not be suitable for all patients.
Sequence of Exercise Execution

- Foot Up and Down: While sitting on a chair, slowly raise and lower your foot. Repeat 10-15 times.
- Circular Foot Movements: While sitting, perform circular foot movements clockwise and counterclockwise. Repeat 10 times in each direction.
- Calf Stretch: Stand and lower the back of your foot onto a small platform or a book, feeling the stretch in your calf. Hold for 20-30 seconds.
- Exercise with Elastic Band: While sitting, fix an elastic band around your foot and pull it toward yourself. Repeat 10-15 times.
- Leg Squeezes (exercise with a ball): While sitting, place a ball between your knees and squeeze it, holding the tension for 5-10 seconds.
- Isometric Quad Tension: While sitting, try to “press” your knee into the floor, holding the muscles in tension for 5-10 seconds.
- Leg Lifts: Lying on your back, slowly raise your leg about 15-20 cm off the floor. Hold for 5-10 seconds.
- Heel Raises: Stand near a wall for support, rise up on your toes, and slowly lower back down. Repeat 10-15 times.
- Sideways Steps: Take several steps to the left and then to the right, holding onto a wall or using a cane for support. Repeat 10-15 times in each direction.
- Partial Squats: Holding onto a chair or wall, slowly squat without going below knee level. Return to the starting position and repeat 10-15 times.
Physiotherapy for Tibia Fractures

In contrast to general exercises, physical therapy (PT) is focused on a more carefully developed and individualized recovery plan. This plan is often developed in collaboration with a physiotherapist and includes not only physical exercises but also various physiotherapy methods. Below are several key components that may be included in a PT plan for recovery after a tibia fracture.
Phases of PT and Their Specifics
- Immobilization Phase: During this period, minimal physical activity is recommended. Exercises primarily focus on reducing swelling and improving blood circulation.
- Mobilization Phase: The beginning of active movements and simple exercises for stretching and strengthening muscles.
- Functional Recovery Phase: Includes complex exercises for coordination, balance, and restoring the full range of motion.
Physiotherapy Methods in PT
- Electrotherapy: Used to alleviate pain and improve microcirculation at the fracture site.
- Ultrasound Therapy: Helps accelerate bone tissue healing.
- Magneto therapy: Used to accelerate the recovery process and reduce inflammation.
Complex Exercises for Functional Recovery
- Pilates and Yoga: Gentle poses and exercises to improve flexibility and muscle strength.
- Hydrotherapy: Water exercises to reduce joint stress.
- Balance Training: Exercises on balance boards to restore coordination.
These methods are often integrated into a comprehensive PT plan, which is developed in collaboration with a physiotherapist and adapted individually for each patient.
How to Avoid Overexertion and Injuries
During the recovery process after a tibia fracture, it’s crucial to avoid additional injuries and overexertion to prevent worsening your condition. Here are some practical tips/recommendations to help you with this:

- Consult with a Physiotherapist: Before starting any physical rehabilitation plan, consult with a qualified physiotherapist.
- Gradual Progression: Start with light exercises and gradually increase the intensity. Sudden increases in intensity can lead to overexertion.
- Warm-Up and Cool Down: Never skip warm-up exercises before starting your workout and cool-down exercises afterwards. This helps prevent muscle spasms and overexertion.
- Proper Technique: Use the correct technique when performing exercises. Incorrect technique not only reduces the effectiveness of the exercise but also increases the risk of injury.
- Listen to Your Body: If you experience pain or discomfort while exercising, stop immediately and consult with a doctor.
- Use Appropriate Gear: Wear proper footwear and use appropriate equipment to minimize the risk of injury.
- Breathing: Correct breathing during exercises can prevent dizziness and fainting.
- Assistance and Supervision: Especially in the early stages of rehabilitation, it’s better to perform exercises under supervision or with the help of a trainer or physiotherapist.
- Regular Rest: Include rest periods between exercises and training days for complete muscle recovery and to reduce the risk of overexertion.
- Hydration: Proper hydration is essential to prevent muscle cramps and spasms, especially during intense physical activity.
- Monitoring Your Condition: Regular medical check-ups and diagnostics to track the recovery process and modify the PT plan accordingly.
By following these tips/recommendations, you can significantly reduce the risk of additional injuries and overexertion, which is crucial for a successful recovery after a tibia fracture.
Additional Rehabilitation Methods for Faster Recovery After a Tibia Fracture
Fast and effective recovery after a tibia fracture requires a comprehensive approach that includes not only traditional treatment methods and physical therapy (PT) but also additional rehabilitation methods. Here are some of them:

- Kinesio Taping: Specialized tapes can support muscles and tendons, reducing strain and accelerating the recovery process.
- Massage and Manual Therapy: These therapies can improve blood circulation, reduce pain, and enhance joint mobility.
- Ozone Therapy: Ozone can improve blood circulation and accelerate the healing of bone tissue.
- Hydrotherapy: Water can serve as a means to reduce pain and improve mobility, while hydromassage can help relax muscles.
- Biofeedback and Electrical Stimulation: These methods can help in pain control and muscle stimulation.
- Acupuncture and Reflexology: These methods may be helpful in reducing pain and improving overall well-being.
- Diet and Nutritional Supplements: Vitamins and minerals such as calcium and magnesium can promote faster bone healing.
- Psychotherapy and Relaxation Techniques: Stress and anxiety can slow down the recovery process. Relaxation techniques and positive thinking can have a positive impact on rehabilitation.
- Individualized Rehabilitation Plan: Working with qualified specialists to develop a personalized rehabilitation plan can significantly accelerate the recovery process.
- Regular Medical Monitoring: Continuous medical supervision and potential adjustments to the treatment plan based on diagnostic results.
These additional methods can complement the primary rehabilitation plan and contribute to a faster and more effective recovery after a tibia fracture.
Nutrition and Supplements Needed to Accelerate Healing of a Tibial Fracture

Proper nutrition and nutritional supplements can significantly accelerate the recovery process of fracture healing and bone tissue restoration. Here are some foods and supplements that are recommended to include in your diet:
Foods:
1. Dairy Products (Cheese, Yogurt, Milk)
Contains: Calcium, Vitamin D
Benefits: Accelerates bone healing, strengthens bone tissue.
2. Salmon and Other Fatty Fish
Contains: Omega-3 fatty acids, Vitamin D
Benefits: Reduces inflammation, improves blood circulation.
3. Nuts and Seeds
Contains: Magnesium, Omega-3
Benefits: Strengthens bones, reduces inflammation.
4. Leafy Green Vegetables (Spinach, Kale)
Contains: Calcium, Magnesium, Vitamin K
Benefits: Strengthens bone tissue, improves blood clotting.
5. Citrus Fruits (Oranges, Grapefruits)
Contains: Vitamin C
Benefits: Stimulates collagen production, essential for bone and tendon healing.
6. Eggs
Contains: Vitamin D, Protein
Benefits: Strengthens bones, maintains muscle mass.
7. Whole Grains
Contains: Phosphorus, Magnesium
Benefits: Strengthens bones, provides energy for overall recovery.
8. Red Meat and Liver
Contains: Iron, Zinc, Protein
Benefits: Improves blood circulation, accelerates tissue recovery.
9. Chicken Broth
Contains: Collagen, Minerals
Benefits: Speeds up bone and tendon healing.
10. Legumes (Lentils, Beans)
Contains: Protein, Magnesium
Benefits: Maintains muscle mass, strengthens bones.
Dietary Supplements:
- Calcium: Strengthens bones and accelerates fracture healing.
- Vitamin D: Enhances calcium absorption.
- Magnesium: Strengthens bone tissue and improves muscle tone.
- Omega-3: Reduces inflammation and enhances blood circulation.
- Glucosamine and Chondroitin: Improve joint and cartilage health.
Before starting any supplements, consult with your treating physician. A comprehensive approach, including proper nutrition and possible use of dietary supplements, can significantly accelerate the rehabilitation process after a tibia fracture.
A tibia fracture is a serious injury that requires a comprehensive and long-term recovery. The right correct approach to rehabilitation will ensure your quick fast and complete recovery.
For a more detailed understanding of the rehabilitation process and exercises, we recommend consulting qualified specialists.

Check out the demo version of our sets of exercises for the Lower Limb Problems on YouTube
Our website presents the following sets of exercises for rehabilitation of the pelvic girdle and hip joint, knee joint and ankle joint:
-
EXERCISES FOR THE PELVIC GIRDLE AND HIP JOINT. SET №1 IS AIMED AT MUSCLE STRETCHING (IMPROVEMENT OF FLEXIBILITY OF THE MUSCULAR APPARATUS) AND INCREASE OF THE RANGE OF JOINT MOVEMENT
-
EXERCISES FOR THE PELVIC GIRDLE AND HIP JOINT. SET №2 IS AIMED AT STRENGTHENING THE MUSCLES
-
EXERCISES FOR THE KNEE JOINT. SET №3 IS AIMED AT STRETCHING THE MUSCLES (IMPROVING THE FLEXIBILITY OF THE MUSCULAR APPARATUS) AND INCREASING THE RANGE OF JOINT MOVEMENT
-
EXERCISES FOR THE KNEE JOINT. SET 4A IS AIMED AT STRENGTHENING THE MUSCLES. INITIAL STAGE
-
EXERCISES FOR THE KNEE JOINT. SET 4B IS AIMED AT STRENGTHENING THE MUSCLES. MID STAGE
-
EXERCISES FOR THE KNEE JOINT. SET 4C IS AIMED AT STRENGTHENING THE MUSCLES. ADVANCED STAGE
-
EXERCISES FOR THE ANKLE JOINT. SET №5 IS AIMED AT STRETCHING THE MUSCLES (IMPROVEMENT OF FLEXIBILITY OF THE MUSCULAR APPARATUS) AND INCREASE OF THE RANGE OF JOINT MOVEMENT
-
EXERCISES FOR THE ANKLE JOINT. SET №6D IS AIMED AT STRENGTHENING OF THE MUSCLES AND IMPROVEMENT OF PROPRIOCEPTION AND STABILITY OF THE ANKLE AND ENTIRE LOWER LIMB. INITIAL STAGE
-
EXERCISES FOR THE ANKLE JOINT. SET №6E IS AIMED AT STRENGTHENING OF THE MUSCLES AND IMPROVEMENT OF PROPRIOCEPTION AND STABILITY OF THE ANKLE AND ENTIRE LOWER LIMB. MID STAGE
-
EXERCISES FOR THE ANKLE JOINT. SET №6F IS AIMED AT STRENGTHENING OF THE MUSCLES AND IMPROVEMENT OF PROPRIOCEPTION AND STABILITY OF THE ANKLE AND ENTIRE LOWER LIMB. ADVANCED STAGE
In addition to the listed sets of exercises please check out article and sets of exercises for the Post-traumatic Rehabilitation of Gait Disorders
Questions and answers
1. How to strengthen bones and prevent fractures?
Regular physical activity, a balanced diet rich in minerals and vitamins, as well as avoiding unfavorable factors such as smoking and excessive alcohol consumption, will help strengthen bones.
2. What are the methods of diagnosing osteoporosis?
There are various methods, such as densitometry (measurement of bone density), X-ray examination, as well as blood and urine tests.
3. What is arthroscopy, and when is it used?
Arthroscopy is a minimally invasive procedure that allows for a visual assessment of the condition of joints. It is often used for the diagnosis and treatment of joint disorders.
4. Is it possible to engage in sports after a fracture?
Yes, but only after complete recovery and with the permission of a doctor. It is usually recommended to start with light loads and gradually increase them.
5. What are the contraindications for physiotherapy?
Acute inflammation, high temperature, malignant neoplasms, and some other conditions may be contraindications for physiotherapy.






