What Is Teenage Stroke?
Updated on May 02, 2024
Medically reviewed by Nicholas R. Metrus, MD
Though most strokes occur in adults ages 65 and older, they can happen at any age. Strokes in teenagers are uncommon, but they are possible.1 When strokes occur in children and teens, it’s usually due to certain underlying health conditions that increase their stroke risk. They face unique challenges after a stroke, as do their parents.
This article discusses the common causes of stroke in teenagers, how they’re treated, and how to cope during the recovery process.
Types of Stroke
There are three main types of strokes. All are possible in teens:2
- Ischemic stroke, the most common type in teens (and adults), is when an artery that supplies blood flow to the brain is blocked. This commonly happens due to a blood clot.
- Hemorrhagic stroke is when an artery in the brain breaks or bursts and bleeds in the brain. This puts pressure on brain cells that damages them.
- Transient ischemic attacks (TIAs), which are sometimes referred to as “mini strokes,” are when blood flow to the brain is blocked for short periods of time. TIAs are considered warning signs of a future stroke.
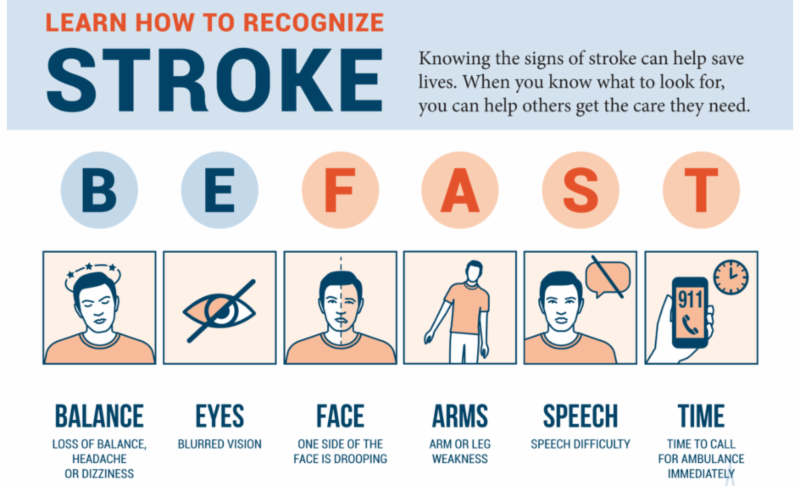
Teenage Stroke Symptoms
Stroke symptoms are the same in teens as they are in adults. The thing is that they may be more easily overlooked in younger people.
It is unusual for a teenager to have a stroke, so the possibility may not immediately come to mind when symptoms arise. In addition, teenagers might not complain about symptoms they are experiencing.
If a teen has any of the symptoms below, get medical attention right away:3
- Severe head pain
- Vision changes
- Weakness
- Confusion
- Slurred speech
- Trouble understanding
- Unusual behavior
- Decreased alertness
- Trouble walking
- Poor balance
- Numbness
- Any sudden change in physical or cognitive function
Causes
If a blood clot forms in or travels to the brain, it causes a stroke.
Certain underlying medical problems can predispose someone to blood clots and stroke. Teenagers who experience stroke often have one or more of these:
- Sickle cell anemia is a hereditary condition that causes blood clots due to a process called sickling, or a change in the shape of red blood cells in response to physical stressors such as infection. About 10% of children with sickle cell experience a stroke.4
- Inborn blood vessel abnormalities such as brain aneurysms, (bulging blood vessels in the brain) and arteriovenous malformations (groups of abnormally connected vessels) may rupture, causing a hemorrhagic stroke.4
- Heart disease or heart malformations can result in an irregular heartbeat, heart function problems, or heart attacks, all of which can lead to stroke.4
- High blood pressure (hypertension), if untreated, can disrupt blood vessels and may cause heart disease or stroke. Hypertension is not common in teenagers and is usually a sign of a medical illness, such as a hormonal imbalance.4
- Infections, especially severe ones, can disrupt the body’s immune system and blood cells to such an extent that increased blood clotting and stroke may occur.4
- Hemophilia is a hereditary blood condition in which the ability for blood to clot is severely reduced, increasing the risk of hemorrhagic stroke.4
- Migraines with aura increases the risk of stroke, and there is a condition called migrainous infarction. These can have similar symptoms as a stroke, and teens who have related symptoms should have a medical evaluation to determine whether they are truly experiencing migraines or whether they are actually having TIAs.5
- Cancer increases the formation of blood clots due to changes in the body’s physiology. Clots are also as a possible consequence of some anti-cancer therapies.6
- High cholesterol is relatively uncommon in teens, but there are some metabolic disorders that can cause elevated blood cholesterol levels. This can lead to heart disease or affect the brain and its blood vessels (cerebrovascular disease).7
- Hormonal changes that occur due to use of hormone therapy, steroids, birth control pills, or during pregnancy can change blood vessel physiology and clotting functions, increasing the risk of stroke.7
- Head trauma, such as a concussion or other head injury, can trigger a disruption in the body that cause either ischemic or hemorrhagic strokes in young people.7
- Drugs and supplements may cause strokes at any age. The use of cigarettes, vaping products, energy drinks, caffeine pills, or illegal recreational drugs are all risk factors for stroke.7
Regular health check-ups in teens can help detect, monitor, and manage any conditions that increase the risk of stroke.
Recap
When a teen suffers a stroke, it is usually due to medical conditions such as a blood disorder, heart condition, infection, or head injury. Medications or recreational drugs can also raise the risk of stroke.
For additional information about the rehabilitation after a stroke you can watch a video demonstrating exercises and rehabilitation recommendations.
A set of exercises for rehabilitation of post-stroke patients. Set No1 is aimed at improving the functions associated with mobility in bed.
Diagnosis
To diagnose a stroke, doctors will take a detailed medical history and run a series of tests that will include brain imaging scans to get a detailed look at the brain.
Tests may include:7
- Blood tests, such as to check for infections or blood clotting disorders
- Magnetic resonance imaging (MRI)
- Computed tomography (CT scan)
- Spinal tap, also called a lumbar puncture, to get a sample of cerebrospinal fluid (what surrounds the spinal cord and brain)
Recap
Symptoms of a stroke in a teenager—severe head pain, sudden weakness, slurred speech, to name a few—warrant immediate medical attention. Brain imaging tests are important in diagnosing stroke.
EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №2 IS AIMED AT IMPROVING THE MOBILITY AND STABILIZATION OF THE PELVIC COMPLEX
Treatment
Treatment for stroke in a teen will depend on the type of stroke and any underlying conditions.
Treatments may include:
- Blood thinners, also called anticoagulants, which are medications used to prevent blood clots from forming or getting larger8
- Thrombolytic medications, intravenous (IV) drugs given through a vein to dissolve blood clots9
- Antibiotics if there is an underlying bacterial infection4
- Anti-seizure medications, also known as anticonvulsants10
- Surgeries, such as to remove a clot, reduce pressure, or stop bleeding in the brain8
- Physical therapy to improve or regain movement and strength11
- Speech therapy to improve or regain verbal abilities11
- Occupational therapy to regain the ability to perform self-directed activities at home or work (e.g., bathing, dressing, eating)11
- Blood transfusions, particularly in those with sickle cell anemia12
A teen who has had a stroke may be referred to a physiatrist, a physician whose expertise is in physical medicine and rehabilitation. This professional can offer or coordinate a variety of therapies.
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №3 IS AIMED AT IMPROVING THE MOBILITY AND FUNCTION OF THE UPPER LIMB, STABILIZING THE SHOULDER GIRDLE
Coping
A stroke in the teenage years can be scary and life-altering, but teens do generally recover more abilities after a stroke than people who are older.4
It can be helpful for both teens and their parents to connect with other teens and families during the recovery process.
The Children’s Hemiplegia and Stroke Association has a support community that hosts in-person and online groups and retreats, and offers therapeutic recommendations.
The American Stroke Association also has a finder tool to help you locate a stroke support group in your area or to find online resources and virtual support.
Recap
Treatments for stroke vary based on the cause of the stroke and its effects. Medications or surgery and rehabilitation therapies are often involved. Support groups for both teens and parents can help with navigating life after a stroke.
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №4 IS AIMED AT IMPROVING THE MOBILITY AND FUNCTION OF THE LOWER LIMB, STABILIZING THE PELVIC GIRDLE
Summary
Stroke in teens is usually caused by medical conditions, such as blood or heart disorders, or drugs that increase the risk of stroke.
Symptoms of a stroke in teens can include severe head pain or sudden vision changes, weakness, confusion, or slurred speech. Teens experiencing symptoms should be evaluated without delay.
The recovery process often involves a series of therapies to try to improve or regain movement, speech, or cognitive abilities affected by the stroke.
By Heidi Moawad, MD
Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.

Demo version of GRS workouts for rehabilitation of post-stroke patients on YouTube
You can find more information about Stroke in our Blog.
Our website presents sets of exercises for the rehabilitation of post-stroke patients in the following four areas:
-
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №1 IS AIMED AT IMPROVING THE FUNCTIONS ASSOCIATED WITH MOBILITY IN BED
-
EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №2 IS AIMED AT IMPROVING THE MOBILITY AND STABILIZATION OF THE PELVIC COMPLEX
-
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №3 IS AIMED AT IMPROVING THE MOBILITY AND FUNCTION OF THE UPPER LIMB, STABILIZING THE SHOULDER GIRDLE
-
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №4 IS AIMED AT IMPROVING THE MOBILITY AND FUNCTION OF THE LOWER LIMB, STABILIZING THE PELVIC GIRDLE
You may also find useful information and sets of exercises in the section APHASIA AND DYSARTHRIA, where 5 sets of exercises for rehabilitation for speech disorders are currently presented.
Sources
https://www.verywellhealth.com/teenage-stroke-3146322
- Centers for Disease Control and Prevention. Stroke facts.
- Centers for Disease Control and Prevention. Types of stroke.
- Cleveland Clinic. Would you know if your child was having a stroke?
- American Stroke Association. Pediatric stroke causes and recovery.
- Gelfand AA, Fullerton HJ, Jacobson A, et al. Is migraine a risk factor for pediatric stroke? Cephalalgia. 2015;35(14):1252-1260. doi:10.1177/0333102415576222
- Tsze DS, Valente JH. Pediatric stroke: a review. Emerg Med Int. 2011;2011:1-10. doi:10.1155/2011/734506
- Singhal AB, Biller J, Elkind MS, et al. Recognition and management of stroke in young adults and adolescents. Neurology. 2013;81(12):1089-1097. doi:10.1212/WNL.0b013e3182a4a451
- Simma B, Höliner I, Luetschg J. Therapy in pediatric stroke. Eur J Pediatr. 2013;172(7):867-875. doi:10.1007/s00431-012-1863-9
- Rivkin MJ, deVeber G, Ichord RN, et al. Thrombolysis in pediatric stroke study. Stroke. 2015;46(3):880-885. doi:10.1161/STROKEAHA.114.008210
- Klučka J, Klabusayová E, Musilová T, et al. Pediatric patient with ischemic stroke: initial approach and early management. Children (Basel). 2021;8(8):649. doi:10.3390/children8080649
- American Stroke Association. The medical rehab team.
- DeBaun MR, Gordon M, McKinstry RC, et al. Controlled trial of transfusions for silent cerebral infarcts in sickle cell anemia. N Engl J Med. 2014;371(8):699-710. doi:10.1056/NEJMoa1401731
Additional Reading
- Boelman C, Shroff M, Yau I, et al. Antithrombotic therapy for secondary stroke prevention in bacterial meningitis in children. J Pediatr. 2014;165(4):799-806. doi:10.1016/j.jpeds.2014.06.013










