A stroke is an acute cerebrovascular accident. This life-threatening condition can occur for two reasons: due to a hemorrhage in the brain or its membranes – such a stroke is called a hemorrhagic stroke or subarachnoid hemorrhage, or if, for one reason or another, blood circulation stops – an ischemic stroke.
It’s important to know! The most common symptoms of a stroke are: sudden weakness (often in one half of the body), facial asymmetry, impaired speech and vision, dizziness, unsteady gait, severe headache, and vomiting.
When such condition occurs, it is extremely important to diagnose it timely, recognizing the symptoms described above and seek a qualified medical care.
To understand what a stroke is, why it happens, and what actions can be taken to rehabilitate and prevent relapses, let’s review the anatomical data.
Anatomical features and the course of a stroke (acute cerebrovascular accident)
A stroke, as mentioned above, occurs in the case of damage to the vessels of the brain. Such a damage may be associated with a vessel rupture or with its blockage. Strokes caused by ruptured blood vessels include hemorrhagic stroke and subarachnoid hemorrhage.
Hemorrhagic stroke
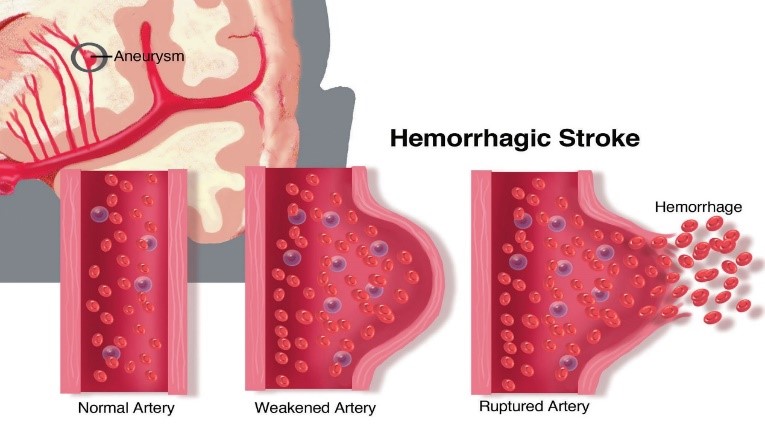
The brain receives the substances necessary for substance functioning with the blood. In order to ensure that in the event of an unforeseen situation, for example, when one of the vessels ruptures or becomes blocked, the brain is minimally damaged, there are several sources of blood supply and a dense network of intertwining vessels (such “plexuses” are called anastomoses). Rupture of cerebral vessels is most often the result of a change in the vascular wall – with atherosclerosis, vasculitis, collagenosis and other hereditary disorders, the vessel wall becomes thinner and loses its elasticity, which can eventually lead to a protrusion of the vessel wall – an aneurysm. In the aneurysm area, the vessel wall is especially thinned, therefore it is easily torn under unfavorable conditions, for example, at increased blood pressure.
When the vessel ruptures, hemorrhage occurs in the brain tissue. Blood compresses parts of the nervous tissue, and the so-called “focal” symptoms occur, the clinical picture of which depends on which part (focus) of the brain was affected. Due to the existence of the system of anastomoses, the pathological process remains localized for some time.
Hemorrhages are classified as parenchymal, when blood from the affected vessel pours directly into the brain tissue and impregnates them; subarachnoid – blood flows into the subarachnoid spaces of the brain; hemorrhage in the ventricles of the brain – this condition is considered by clinicians to be the most severe; and also there are mixed forms of hemorrhages.
Compared with ischemic stroke, hemorrhagic stroke has a more acute onset, it develops more often during the daytime against the background of stress, physical or emotional stress and is accompanied by a sharp increase in blood pressure, which leads to rupture of cerebral vessels.
Ischemic stroke
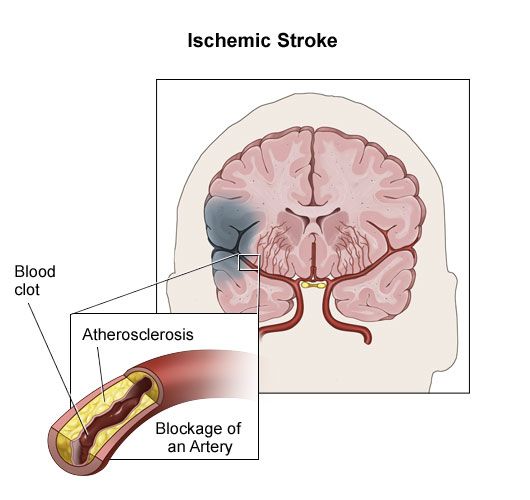
Ischemic stroke, like hemorrhagic stroke, is characterized by an acute damage of cerebral circulation, which, however, occurs not due to rupture of cerebral vessels, but due to their blockage.
The most common cause of ischemic stroke is atherosclerosis.
Atherosclerosis is characterized by cholesterol deposition on the inner wall of the arteries, the formation of atherosclerotic plaques, narrowing of the lumen of vessels and, as a result, a decrease in blood flow. The brain begins to receive less nutrients and oxygen, and in the case when the lumen of the supply vessels narrows critically, an ischemic stroke occurs.
Ischemic stroke, blood clot, atherosclerosis
A critical decrease in blood flow in the case of ischemic stroke occurs as a result of:
-
Thromboembolism – a vessel blockage by a thrombus or atherosclerotic plaque that has come off the vessel wall as a result of increased blood turbulence (increased blood pressure).
-
Vascular spasm.
Ischemic stroke is characterized by the disease development at night.
hemorrhagic and ischemic strokes Symptoms
Both hemorrhagic and ischemic strokes are characterized by three groups of symptoms that are important to distinguish for the timely diagnosis of the disease.
Focal symptoms
Focal symptoms in a stroke occur first. They appear because a certain part of the brain is affected. The disease symptoms that occur first are explained by the dysfunction of the affected area.
A good example of focal symptoms is hemiparesis – muscle weakness in the arm and leg of the affected side. When the region of the brain responsible for the ability to move in one half of the body is affected, its functions suddenly “turn off”, and therefore the ability to fully move in the limbs is also lost.
Other examples of focal symptoms include:
- Face distortion, drooping of the mouth corner
- Visual impairment – hemianopsia – loss of the ability to see with the right or left halves of the eyes.
- Speech disorder – APHASIA AND DYSARTHRIA – the impaired ability to speak and understand speech.
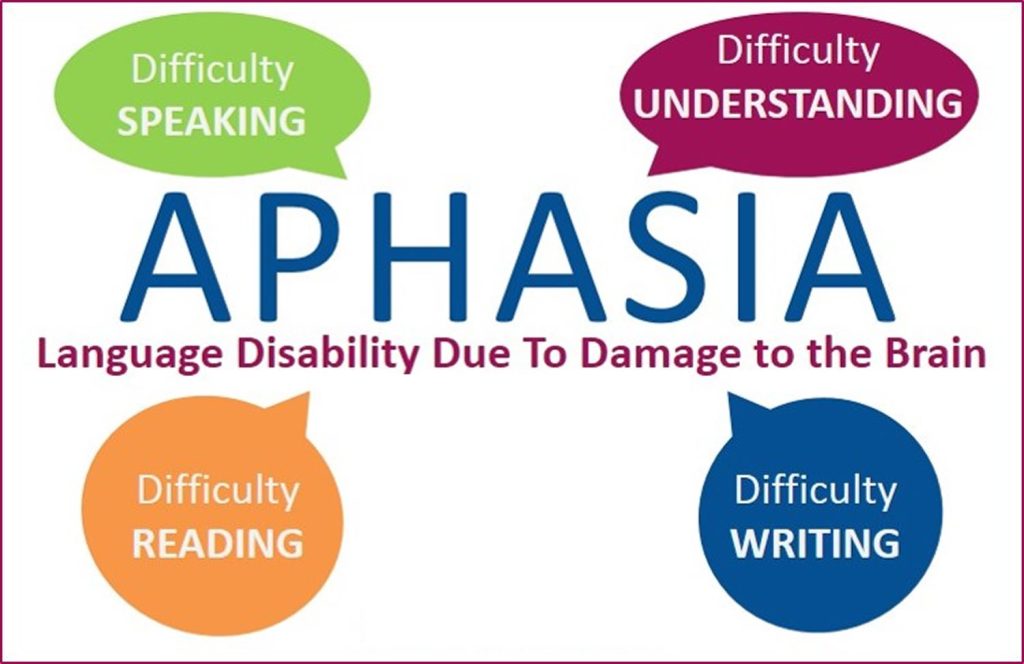
APHASIA most often with a stroke, a patient develops total aphasia. This is an impairment of the motor and sensory link of speech. The impairment of the motor link is manifested by a patient’s loss of the ability to normal speech, he speaks very slowly, in separate phrases, sounds, and sometimes is not capable of speech at all. The impairment of the sensory link is related to speech perception: a patient does not understand the addressed speech, does not understand what any conversation is about.
DYSARTHRIA – an impairment of speech pronunciation. Such a disorder is related to the impairment of the innervation of the facial muscles responsible for speech formation. Dysarthria is manifested by slurred, fuzzy speech “into the nose”, salivation. Speech is quiet, deaf, monotonous.
- Unsteady gait, loss of balance.
- Dizziness.
Focal symptoms at the disease onset are typical ischemic stroke.
General cerebral symptoms
General cerebral symptoms are represented by headache, nausea, vomiting; impaired consciousness may develop: from stupor to coma.
Sudden cerebral symptoms at the disease onset are typical of hemorrhagic stroke.
Meningeal syndrome
The meningeal symptom is otherwise called membranous and manifests itself with hemorrhage in the brain membranes, that is, with subarachnoid hemorrhage. Symptoms of meningeal syndrome are hypersensitivity to sounds, light, touch; neck stiffness (it is felt when trying to bend the head to the chest).
the risk factors for stroke
It is important to mention the risk factors for stroke. They include:
-
High cholesterol
-
Hypertension
-
Diabetes
-
Cardiac disease
-
Sedentary lifestyle/Professional sports
-
Overweight
-
Age (45+ for hemorrhagic stroke, 60+ for ischemic)
-
Social habits: smoking, drug addiction, alcoholism
-
Blood disorders: blood clotting disorders
-
Transient ischemic attacks
-
Sleep Apnea
-
Previous stroke, heart attack, or TIA
-
Vascular diseases
Treatment and rehabilitation after stroke

Stroke treatment consists of emergency care and a long rehabilitation process.
Emergency care for stroke patients is provided by qualified specialists. They have the task to lowering blood pressure smoothly, maintain adequate oxygenation and hemodynamics. The following drugs are prescribed: analgesics for pain, antiplatelet agents and anticoagulants to reduce the risk of thrombosis, sedatives, etc.
After the acute period, a patient will have a long rehabilitation period. The rehabilitation process begins at the patient’s bedside and is managed by qualified specialists from a multidisciplinary team – post-stroke rehabilitation is especially effective when it covers several areas: physiotherapy, speech therapy and occupational therapy.
Rehabilitation after a stroke is carried out comprehensively, in several stages for the gradual restoration of functions and the return to a normal full life.
What does the rehabilitation process after a stroke include?

Rehabilitation usually includes physical therapy, occupational therapy, psychological consulting, support from social workers, etc. The main goal is to return to the level of functioning that was before the stroke as much as possible.
Rehabilitation methods
Rehabilitation methods include such methods as:
-
Passive kinesiotherapy – movement therapy, a complex system of exercises using special devices.
-
Physiotherapy.
-
Manual therapy, massage.
-
Ergotherapy or occupational therapy – is indicated for the restoration of everyday functions, helps a patient to restore lost skills, including fine motor skills.
Rehabilitation after a stroke is individual and depends on the nature and extent of the damage.
Physiotherapy rehabilitation complexes for patients with previous stroke can be divided according to the degree of injury:
When an injury is mild, the rehabilitation process helps to improve all daily functions and regain maximum independence.
For moderate injuries, the importance of physiotherapy is to preserve as much of the existing ones as possible and improve the performance of daily functions and mobility.
In case of a severe injury, the goal of physiotherapy and long-term planned rehabilitation is to maintain the existing functional activity and ability, prevent complications such as contractures and bedsores, and ensure patient comfort and the best possible quality of life.
Rehabilitation plan
When forming a rehabilitation plan and developing a system of exercises, it is necessary to take into account numerous aspects and emphasize and focus mainly on:
Strengthening muscle strength with an emphasis on the shoulders, arms and legs.
Improve cardiopulmonary endurance as well as muscle stamina so you can train and stay active longer.
Increased flexibility and mobility with a focus on the spine and limbs to maintain joint range of motion and reduce pain.
Improve hand function and fine motor skills: Through various exercises, the tone of the hands can be reduced and the ability to use the hand in daily life can be improved.
Daily functional exercise: muscle weakness or increased tone, problems with coordination, balance and problems with planning, over time cause difficulties in daily activities. Difficulty can be expressed in walking, standing, sitting, rolling in bed, getting up, getting dressed, and more. Therefore, it is very important to perform exercises, the purpose of which is to improve daily motor functional activity. Multiple repetitions improve performance and function.
Improved walking and mobility: Maintaining the ability to walk and mobility is very important for daily functioning and independence. Due to muscle weakness, lack of flexibility, reduced cardiopulmonary endurance, imbalance and difficulty in planning movements, neurological patients experience difficulty walking. With the help of a rehabilitation specialist, you can learn techniques that improve gait and walking ability, as well as explore the need for using walking aids. If the health condition does not allow walking, the possibility of independent mobility with the help of a suitable wheelchair should be explored.
Fall Prevention: Many patients report falls and stumbling. Having fear of falling, they sometimes tend to avoid activity and walking, and, correspondingly, have body weakness and a further deterioration in balance. Therefore, it is important to include exercises in the rehabilitation program to improve balance, coordination and balance.
The plasticity of the nervous system
For the correct forming and planning of the rehabilitation process, it is it is very important to understand and explain what is cerebral neuroplasticity.
Neuroplasticity, nervous system plasticity, or “brain flexibility” refers to the ability of the brain to change in response to emotions and experiences. Plasticity is what allows the nervous system to adapt its activities to changes in the environment. Essentially, it is the ability of the brain to reorganize itself in response to our everyday experience. This plasticity is basically a learning process. At the cellular level, plasticity occurs due to real changes in the connections between neurons and changes in the design of synapses. That is, the brain does this by strengthening some synapses and weakening others.
In the past, it was believed that changes in the brain occur mainly in childhood before the age of 20. Since the 1960s, more and more evidence has accumulated that learning and cerebral plasticity can occur throughout life.
The plasticity of the nervous system is of fundamental importance in the processes of neurological rehabilitation
Neuroplasticity is a key tool in the rehabilitation process. For example, after a stroke, in which entire areas of the brain are actually damaged. In such cases, there is a more extensive process of synaptic changes in which whole areas and functional units of the nervous system change their functions and patterns of activity. It is very important to emphasize that plasticity depends on real life experience, depending on the environment and the variety of activities. Therefore, plasticity can be indeed improved with the help of physical activity, practice and real rehabilitation processes.
Just as a person at the age of 30 can start learning to play the guitar and, through intensive practice, he will continue to improve, so the process of intensive rehabilitation will help to acquire new abilities and compensatory skills.
With the right stimulation, we can stimulate neuroplasticity in the brain and thus strengthen the synapses in the brain. Changes in the brain can be so significant that new synapses form, and certain areas of the brain can “take over” the role of damaged areas.
How to increase brain neuroplasticity stimulation after a stroke?
In order to induce real changes in the brain and stimulate neuroplasticity after a stroke, one needs to practice a lot and carry out an intensive and focused rehabilitation process with many repetitions of daily activities and functions, sometimes with the help of a physiotherapist or a rehabilitation therapist having extensive experience in neurological rehabilitation.
Video: “Rehabilitation after a stroke”
A set of exercises for rehabilitation of post-stroke patients. Set No1 is aimed at improving the functions associated with mobility in bed.
For additional information about the rehabilitation after a stroke you can watch a video demonstrating exercises and rehabilitation recommendations.
principles that should be followed in the process of rehabilitation after a stroke
What are the principles that should be followed in the process of rehabilitation after a stroke, and contributing to the development of neuroplasticity:
Principle “use it or lose it”
Principle “use it or lose it” meaning “use it so as not to lose it”. It means that all the skills that we stop using will disappear. For example, using a weak hand: if a person stops using a weak hand after a stroke, the synapses responsible for the function of the hand weaken, die, and eventually the hand will not be able to function at all.
Principle “use and improve”
Every action we take can be improved. Following the example of using a weak hand, if a person touches the hand, uses it more, first tries to use it as a “helping hand”, then increases activity – he strengthens the responsible synapses and further sees an improvement.
Principle of repetition
n order to achieve improvement, the same task should be repeated again and again. This repetition strengthens the synapses and can eventually cause changes in the brain.
Principle of intensity
Multiple repetitions, with high frequency, several hours a day. Recent studies have shown that you need to train even several times a day to create changes in synapses
Principle of specificity
In order to improve a specific task, it is necessary to practice it specifically and its components. For example, in order to improve walking after a stroke, it is necessary to practice certain elements of walking and walking itself. To improve walking, you should work on various components that are important for walking, such as: improving balance, strengthening leg muscle strength, improving the range of motion of the foot, knee and hip, practicing walking on different surfaces, indoors and outdoors, picking up a walker or stick for safe walking and much more. Standing alone and exercising will not lead to improved gait…
Principle of significance
One of the most important principles of any rehabilitation process is that the performance of exercises and tasks should be meaningful, consciously desired and relevant for any patient. This is necessary to mobilize cooperation and motivate any patient. Stroke rehabilitation needs to be meaningful and relevant to get the most benefit out of it.
Bobath therapy
One of the most effective rehabilitation systems is Bobath therapy. This technique was developed by British specialists Bertha and Carl Bobath in 1943.
In the Bobath concept, the human body is considered as a single system, where all muscles and tissues are interconnected. And by acting on a healthy part of the body, you can gradually restore the mobility of the affected one.
Exercises are aimed at reducing excessive muscle tension (tone). The method is based on stretching the extensor muscles. The course of therapeutic gymnastics provides a wide range of exercises for stretching and strengthening muscles in order to restore sensitivity and self-control of the body, restore maximum functional activity and ability.
Patient’s recovery after a stroke is based on constant interaction with a rehabilitation specialist.
Bobath therapy makes it possible to restore motor activity, using the plasticity of the nervous system.
Bobath therapy is an effective method not only for post-stroke recovery, but also for the treatment of diseases such as:
-
Cerebral palsy
-
Delayed psychomotor development
-
Spasm of limbs
-
Movement and balance disorders
-
Multiple sclerosis.
With all these diseases, the use of Bobath therapy allows you to improve the quality of motor activity over time.
Neuro-Integrative Functional Rehabilitation | NEURO-IFRAH
Another effective modern method of rehabilitation after a stroke is the NEURO-IFRAH method (Neuro-Integrative Functional Rehabilitation). This method was developed by Waleed Al-Obudi. It is aimed at the comprehensive restoration of physical, mental, social, professional and economic status. During treatment, patients reacquire lost skills and learn new ones.
There are many variables that need to be considered for successful rehabilitation, recovery and resumption of life roles. “Body movements are somewhat like the letters of the alphabet. The possible combinations of body movements are a lot like words. Knowledge of the body, knowledge of all other systems, knowledge of the patient, knowledge of the trauma, knowledge of the environment and knowledge of many other variables is the key to successful rehabilitation,” is the concept of the program developers.
The combination of timely diagnosis of a stroke, competently provided emergency care and a recovery program after a stroke prescribed by a rehabilitation specialist allow you to gradually restore the patient’s lost functions, return to a full life and minimize the risk of relapse of the disease.
To prevent a stroke, it is necessary to establish a healthy diet, minimize the amount of animal fats and salt, avoid stress, give up social habits, and lead an active life style.

Check out the demo version of our workouts for rehabilitation of post-stroke patients on YouTube
Our website presents sets of exercises for the rehabilitation of post-stroke patients in the following areas:
-
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №1 IS AIMED AT IMPROVING THE FUNCTIONS ASSOCIATED WITH MOBILITY IN BED
-
EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №2 IS AIMED AT IMPROVING THE MOBILITY AND STABILIZATION OF THE PELVIC COMPLEX
-
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №3 IS AIMED AT IMPROVING THE MOBILITY AND FUNCTION OF THE UPPER LIMB, STABILIZING THE SHOULDER GIRDLE
-
A SET OF EXERCISES FOR REHABILITATION OF POST-STROKE PATIENTS. SET №4 IS AIMED AT IMPROVING THE MOBILITY AND FUNCTION OF THE LOWER LIMB, STABILIZING THE PELVIC GIRDLE
You may also find useful information and sets of exercises in the section APHASIA AND DYSARTHRIA, where 5 sets of exercises for rehabilitation for speech disorders are currently presented.