Pain in the lumbar region is familiar to every person, as it significantly affects vital activity and the ability to perform daily activities. 80% of the world’s population has experienced or will experience pain in the lumbar spine at least once in their lives. Back pain is the most common reason for visiting orthopedic specialists and neurologists for medical care. For example, recently, the budget allocated for medical needs related to back pain has been more than $50 billion. Pain in the lumbar spine is specific (when the cause and origin are known) and accounts for only 15% of the total. In 85% of cases, pain is defined as non-specific and is called “non-specific lower back pain” (NSLBP). In men, lumbar pain is manifested more often (2 times) compared to women.
Lower back pain can be caused by a variety of factors – from physical fatigue to various pathological processes in the spine, therefore, if this symptom occurs, it is necessary to consult a qualified specialist in order to establish an accurate diagnosis and prescribe the appropriate treatment.
Pains in the lumbar region can be completely different in nature: they can appear suddenly and be acute, or they can increase gradually, developing from barely perceptible to severe.

Lower back pains are divided into types and mechanisms of origin:
-
Punctual pains (centralized) – mostly discogenic in nature
-
Lateral pains, left or right, due mainly to muscle structures.
-
Irradiating pains radiating to the buttocks and limbs, due to pressure on the nerves.
Let’s consider in more detail the causes of pain in the lumbar region. Back pains, regardless of the originating cause, share increasing in symptoms of discomfort after a long stay in a certain position, for example, when sitting or standing. It will be difficult for any patient to sit or stand up, the condition may be accompanied by spasms of the back muscles, pelvic and hip stiffness. In some cases, patients may feel tingling and numbness, creeping sensations that occur when adjacent nerves are involved in the process.
First of all, to clarify the causes of back pain, a comprehensive diagnostics is required. Correct and timely treatment of any diseases will ensure a faster recovery and reduce the possibility of relapses. Fortunately, in most cases, an effective way to treat pain in the lumbar spine lies in conservative methods: physiotherapy, massage, manual therapy and exercise therapy. These methods, if prescribed by a qualified specialist, can significantly improve a patient’s quality of life, and eventually forget about pain altogether.
In order to understand the causes of pain in the lumbar region, let’s review the features of the anatomical structure of this region.

Anatomical particularities of the lumbar spine
The lumbar spine consists of 5 vertebrae. Unlike the vertebrae in other parts of the spine, the lumbar vertebrae are the most massive. This is due to the fact that the lumbar region, in a certain sense, is the foundation of the entire spine and experiences the greatest load, allowing a wide range of movements. Although this part of the body is well designed, it is prone to injury. So, for example, due to the high load on the lumbar vertebrae, they are among the first to undergo pathological changes in age-related diseases such as osteoporosis or spondylarthrosis. The same load, but in other conditions, for example, in the gym, when lifting heavy weights, can also lead to muscle strain, damage to the spine, and sometimes fractures. Due to the peculiarities of human behavior while falling, injuries of the lumbar vertebrae are quite common – bruises and fractures are often the cause of a visit to a traumatologist.
Between the bodies of two adjacent vertebrae are intervertebral discs – cartilaginous structures that provide strong adhesion, flexibility, mobility and cushioning of the spinal column. Intervertebral discs are made up of two main components: first, a ring-shaped structure called the annulus fibrosus. It provides cohesion and integrity of the structures of the spine. Inside the fibrous ring is the nucleus pulposus. It consists of a gel-like mass, which allows you to provide shock-absorbing functions of the intervertebral discs. On both sides of the intervertebral disc, between it and the body of the upper and lower vertebrae, there are hyaline plates that maintain the integrity of the structure.
Intervertebral discs are more prone to degenerative changes than other structures of the spine. This is due to the fact that their metabolic processes are very slow. Due to the deficiency of minerals and a decrease in fluid amount – dehydration, the nucleus pulposus may lose its elasticity, and consequently, its shock-absorbing function. A very large percentage of people suffer from such changes, especially those over 30 years old. The changes result in the development of osteochondrosis, as well as protrusions or hernias of the intervertebral discs, which will be discussed below. In young people under 30 years of age, the intervertebral disc is soft, flexible, elastic, and serves as a shock absorber for the spine. With the age of over 30 years, it loses flexibility, elasticity, due to changes in the structure of soft tissues and collagen fibers. It should be noted that sometimes disc herniations are asymptomatic and are not accompanied by a characteristic clinical picture.
In most cases, damage to the intervertebral disc occurs due to the increased pressure for one reason or another. Repetitive movements associated with the body rotation, lifting heavy objects, as well as improper loading – mainly contribute to intervertebral hernias and pathological syndromes associated with incorrect posture and aggravation of lumbar pain.
The disc prolapse can occur as a result of an injury, for example, in an accident or a fall from a large height, or during degenerative changes, when the disc nutrition is impaired, and at the same time, its strength and elasticity are lost (for example, when sitting for a long time) One of the complications of such changes of intervertebral disc is the formation of a hernia.
Four stages of the formation of an intervertebral hernia
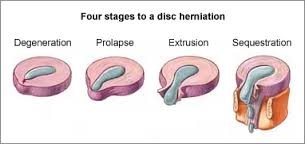
A herniated disc is formed when the integrity of the fibrous membrane is impaired, and the disc goes beyond the boundaries. The figure above shows the four stages of the formation of an intervertebral hernia.
Stage 1 – degeneration or protrusion
At this stage, a gradual deformation of the disc tissues is formed, the structures still retain their integrity, but their boundaries begin to shift. Most often, this stage is not accompanied by any symptoms and may be an incidental finding during a medical examination.
Stage 2 – prolapse
At this stage, a deeper displacement of tissues occurs, the nucleus pulposus loses its shape and spreads beyond the fibrous ring of the disc, gradually starting to compress adjacent spinal fibers. Mild nagging pains appear, which are easily confused with the symptoms of spondylarthrosis – they occur after physical exertion and do not cause much discomfort.
Stage 3 – extrusion
At this stage, the integrity of the fibrous ring is broken, and the nucleus pulposus goes beyond it. As a rule, the moment of rupture itself is associated with a dramatic axial load on the spine and is accompanied by a sharp shooting pain, which gradually subsides, leaving behind a limitation of mobility and swelling of the soft tissues. This condition usually leads patients to a physician, where they are prescribed appropriate therapy, including pain relief, elimination of nerve root compression and a course of specially selected exercises, physiotherapy and traction (stretching) of the spine. Such complex therapy makes it possible to strengthen the musculoskeletal apparatus of the lumbar region and not only prevents relapses, but also formation of new intervertebral hernias.
Stage 4 – sequestration
At this stage, part of the hernial protrusion separates from the disc and dies, while remaining in the tissues. The human immune system reacts to its own necrotic tissue as if it were a foreign body, resulting in inflammation. This condition can cause intense pain, severe impairment of motor activity, severe swelling, the patient needs a qualified medical care, which most often consists of surgical intervention. In order not to aggravate a situation, it is necessary to contact a specialist in time.
The pectoral girdle corset of the vertebral region provides a reliable protection of the musculoskeletal system and internal organs from harmful effects of excessive loads. The muscles in this area are divided into two layers – superficial and deep.

Particularities of the biomechanics of the lumbar spine
As for biomechanics, the lumbar spine located between the mobile thoracic region, on the one hand and the inactive pelvis, on the other, performs two functions at once: static and dynamic.
Static function is the resistance to loads and transmission of power impulses, while the dynamic function provides a wide range of motion.
Taking into account the above features of the anatomy of the lumbar region, it is easy to understand which of the elements are responsible for the performance of motor function. These include muscles, intervertebral discs (we have mentioned that they provide shock-absorbing action and flexibility of the spine), and the articular surfaces of the facet joints between the vertebrae.
Physiologically, the lumbar spine is characterized by lordosis – the bending of the spinal column, in which the bulge is turned anteriorly. This structure of the region is of biomechanical significance – in a static position, lordosis increases resistance to excessive pressure, thereby reducing the load on the intervertebral discs and thereby preventing their degeneration. That is why maintaining the physiological curves of the spine is so important.
What are the main causes of pain in the lumbar spine:
Degenerative changes in the vertebrae
Degenerative changes in the vertebrae and facet joints of the spine often affect the intervertebral discs, as well as the roots of the spinal nerves that go out into the holes between the two vertebrae. Damage to the bone and cartilage structures of the musculoskeletal system, namely the vertebrae and intervertebral discs, may be the result of a decrease in the strength of the vertebrae as a structure, resulting from age-related functional changes.
Already at the age of 20 to 40 years, there are slight changes in the vertebrae, cartilage and articular surfaces erasure. This leads to the initial stage of degeneration of the intervertebral discs and joints. This is usually accompanied by possible back pain, which in 90% of cases can resolve spontaneously.
At the age of 40 to 60 years, more serious structural changes occur associated with subluxation of the vertebrae and the manifestation of disc herniations, more pronounced pain in the lower back (“grabbed the back”), as well as irradiation of pain in the leg. Disc herniation is the most common and frequent type of disorder in this case.
At the age of over 60 years, the main problems appear – narrowing of the spinal canal (stenosis). In this case, there are severe pains in the back and legs that interfere with walking, daily functions, and there may also be neurological manifestations – decreased sensitivity and impaired motor function of the lower extremities.
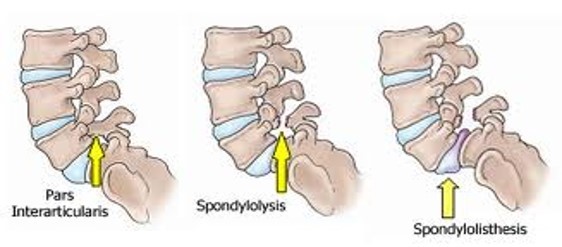
Severe changes in the discs can lead to such a phenomenon as hypermobility of the vertebrae in the lumbar region. An additional problem may be the impairment of the normal vertebral mobility (increased stiffness in other vertebrae), and thus an imbalance in the lumbar region leading to an increase in pain and its transformation into chronic pain. Since the discs are known for poor blood supply, there is a slowdown in their restoration and recovery processes. An increase in instability (increased movement) in one vertebra, and a decrease in mobility (stiffness) in another, loss of control of the underlying muscles over the spinal column can cause stress fractures as a result of loads, even not very significant ones (most often, L4-L5). This condition is called spondylolysis. If the condition worsens, and one vertebra slips in relation to another, then such a process is called spondylolisthesis which is aggravated by degenerative processes in the disc itself. There is a great danger of spinal stenosis (narrowing of the spinal canal), which can lead to irreversible consequences and requires surgical intervention.
A special method and a set of exercises aimed at strengthening the core muscles in the pelvic girdle, lumbar region and increasing very important processes of improving the stability of the lumbar vertebrae and reducing imbalance have been developed.
Pain of muscular origin
The most common cause of pain in the lumbar region (90%) is pain of muscular origin.
Often, when a patient complains of a “grabbed back”, a pronounced muscle spasm or so-called trigger points in the core postural muscles are found, sometimes there is stretching or damage to the muscles located in this area.
As a result, pain occurs, which can sometimes last up to several weeks without proper medical attention.
The muscles of the lumbar region are divided into two groups: superficial and deep. The superficial muscles include the external oblique muscle of the abdomen and the latissimus dorsi muscle. Deep muscles include the internal oblique muscle of the abdomen, serratus muscles, the square muscle of the lower back and the muscle that straightens the spine. Most of the back muscles are extensor muscles, they keep the spine in a straight position, while the abdominal muscles, for the most part, are stabilizing and perform actions that require tilt.
It is quite easy to stretch or injure the muscles of the lumbar back. Common reasons include:
- Sharp lifting of weights
- Sport injuries
- Activities that cause sudden excessive stress on the lower back, such as a fall
- Long-term maintenance of an incorrect posture or position can lead to a chronic load to the muscles of the lower back, as a result of which the muscles will be in good shape at first, and over time their reserves will run out and they will gradually weaken.
Now we should mention the Low Crossed Syndrome (LCS)
As with the upper crossed syndrome, lower crossed syndrome or LCS is caused by muscle imbalance resulting from a sedentary lifestyle and poor posture. With this syndrome, there is tension in the muscles that flex the hip and muscles that extend the lower back, as well as weakness of the deep abdominal muscles and gluteal muscles. Thus, a patient suffering from the lower crossed syndrome will look like this: his stomach will protrude forward due to an overly arched lumbar back, the muscles of the lower back and gluteal region will be in constant tension, there will be a feeling of stiffness. Prolonged contraction of the muscles of the above areas, as well as the groin and thighs, will cause a constant aching pain, which intensifies in the evening, as well as after physical exertion.
The lower crossed syndrome should not be neglected, its chronic course can significantly slow down any rehabilitation process or cause complications on nearby joints, which sooner or later will lead to a deterioration in their functions, and therefore to a loss of the ability to move freely. An effective method of treatment of the lower crossed syndrome is physiotherapy, manual therapy, the development by a specialist of an individual set of exercises aimed at strengthening the pectoral girdle of the lumbar region, on the one hand, and relaxing overly tense muscles, on the other, as well as the anterior capsule of the hip joint.
Pains of neurological origin
The next reason is pains of neurological origin, as a consequence of pressure of the intervertebral disc on the nerve or narrowing of the intervertebral foramen, which also creates pressure on the outgoing nerve, causing a local swelling and inflammation, which increases pressure on the nerve trunks. This type of pain is called radicular or radiating, when the patient complains of pain irradiating to the leg.
Damage to the spine joints
Lumbar spondylarthrosis is a chronic disease characterized by damage to the facet joints of the spinal column. There are many reasons for this condition. Orthopedic experts say that one of the most common causes of spondyloarthrosis is overweight, as a result of which the constant load on the lower spine increases and eventually leads to degeneration. Among other reasons: spinal injuries, heavy physical exertion, elderly age. Women are more susceptible to this disease than men.
Due to the above factors, the pressure on the spine increases, and the intervertebral discs, which normally support depreciation, flatten over time, as a result of an uneven distribution of the load in the joints, inflammation develops.
The main symptom of lumbar spondyloarthrosis is aching pain, which at the initial stages occurs during physical activity, and over time it begins to disturb even at rest, interfere with restful sleep, and does not allow you to perform freely normal actions.
In most cases, the disease does not require radical treatment, and conservative methods of therapy are used. Massage and physiotherapy exercises which facilitate the disease course and slow down its progression play the most important role.
Other sources
Pains not related to the musculoskeletal system. Such as: internal organs that radiate to the lower back, for example, renal problems; oncological problems (often metastases are concentrated in the lumbar spine); spinal inflammation, compression fractures resulting from osteopenia and osteoporosis, and degenerative changes common with age.
Posture impairment
Posture impairment, muscle imbalance related to a sedentary lifestyle, decreased physical activity, manifested in prolonged sitting (at work, at the computer, prolonged traffic jams, long trips, etc.). It should be noted that in this regard, the so-called “rejuvenation” of the lumbar pain is of more and more concern to specialists. It manifests itself in the younger generation, already starting at the age of 12-14 years.
Prolonged sitting position leads not only to a large load on the vertebral discs, their erasure and degeneration, but also to various musculoskeletal disorders, and various syndromes that affect back pain. (e.g. LCS)
Smoking
Many studies have proven a direct relationship and correlation between smoking and back pain, since smoking constricts blood vessels and reduces the nutrition of intervertebral discs, which are anatomically very poor in blood supply.
Malnutrition and overweight
Malnutrition and overweight is also a common cause of back pain.
Incorrect or long-term inadequate posture
Chronic pain related to an incorrect or long-term inadequate posture – so, for example, improper ergonomic equipment of the working place in which a person is located throughout the working day.
Psychological factors
It is very important to mention psychological factors, being the reason of the lumbar pains. Recently, more and more studies have shown the importance of a psychological condition that causes pathology and back pains.
Nervous stress, constant tension at work, dissatisfaction with life and working conditions, family strains, unsettledness, constant concern are additional factors that negatively affect developing back pains.

Treatment of back pain
By the time of occurrence of lumbar pains, they can be classified in accordance with three periods:
-
Up to 3 weeks – acute stage / acute period
-
From 3 to 6 weeks – subacute / subacute stage
-
Over 6 weeks – chronic
A different attitude towards these periods, understanding the nature of the origin of back pain will be the main factor in the development of programs and sets of physical exercises and instructions for the main actions in everyday life.
How to treat? Treat back pain like a disease, or….
For many years, the main recommendation of orthopedists for acute low back pain was bed regime and rest. But in recent years, this view has changed dramatically. Many studies have shown that mobility and activity, especially in the first, acute period, helps to reduce pain. Physical activity and exercise are particularly effective in the long term for reducing pain, improving functions of daily living, improving quality of life, while emphasizing the preventive function of exercise in preventing further progression of low back pains. Therefore, it is important to observe a stepwise, gradual return to normal functioning, preferably relying on instructions of a therapist or instructor. It is very important to choose physical exercises and develop guidelines for physical activity individually, after a detailed check by a specialist – a doctor or a physiotherapist. Not everything that suits one patient may suit another.
Guidelines and directives of the World Organization of physiotherapists and rehabilitation physicians
The main guidelines and directives of the World Organization of physiotherapists and rehabilitation physicians in relation to low back pain at the moment are:
-
Early return (prevention of bed regime and passive rest, as well as lying on a board) to movement and at least minimal activity, being extremely attentive to the level of exertion, avoiding sharp movements and selecting minimal activity that is not related to pain sensations.
-
Warming up the muscular apparatus helps to reduce pain. It can be done using devices for warming up and warming ointments.
Multidisciplinary approach to the treatment of the low back pains
During treating low back pains, it is necessary to take into account the integrated multidisciplinary approach, including:
-
Posture improvement.
-
Improved movement and physical activity (adequately corrected)
-
Increasing the flexibility of the musculoskeletal system.
-
Muscle strengthening.
-
Improvement of endurance.
-
Return to exercise and physical activity, preferably under the guidance of a specialist.
-
Development of a home exercise program to maintain the effects of treatment in the long term and prevent the recurrence of herniated discs and back pain.
-
Ergonomy and arrangement of the working place.
-
Correct nutrition and weight loss.
-
Stop smoking.
-
Adequate attitude to psychological problems.
Supervision of a qualified specialist
Any acute pathological process should be treated under the supervision of a qualified specialist. At the acute disease stage, it is very important not to harm the body, therefore and it is necessary to select the minimum activity that is not related to occurrence of pain. However, the treatment of non-acute lumbar diseases requires a patient’s active participation.
Video: “Exercises for the Rehabilitation of Lumber Spine problems”
Lumber Spine: Set No1 General rehabilitation and support. Initial stage.
For additional information about exercises for the rehabilitation of Lumber Spine problems you can watch a video demonstrating exercises and rehabilitation recommendations.
Physiotherapy
One of the most effective ways to treat lumbar spine diseases are physiotherapy, manual therapy and physical therapy. Only a set of exercises correctly selected by a specialist in combination with physiotherapy will ensure a rapid recovery and return to an active life.
In physiotherapy, exercises aimed at stabilizing the lumbar spine are actively used. The purpose of these exercises is to strengthen the pectoral girdle and core muscles which help to keep the spine in a healthy position, in the long term, it solves the problem of back pain. Stabilization methods include exercises to improve the flexibility, strength, and endurance of the spine. A special system and set of exercises have been developed to improve the stabilization of the lumbar vertebrae and prevent surgical intervention.

Check out the demo version of our sets of exercises for Lumbar spine on YouTube
Our website presents the following sets of exercises for the lumbar spine:









